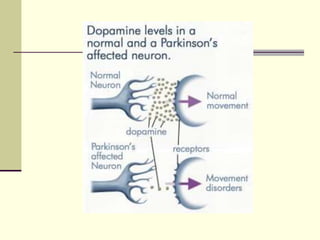
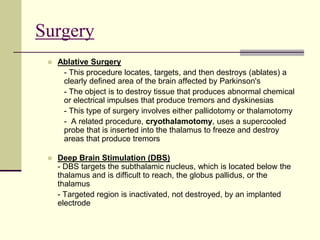
Parkinson's disease is a progressive neurodegenerative disorder characterized by loss of dopaminergic neurons. Its primary symptoms include tremor, rigidity, slow movement, and impaired balance. While medications can provide symptomatic relief, there is no cure. Physical therapy focuses on improving mobility, balance, strength, and fall prevention through exercises like treadmill training, Tai Chi, stretching, and cueing strategies. Surgery such as deep brain stimulation may also help manage severe symptoms.