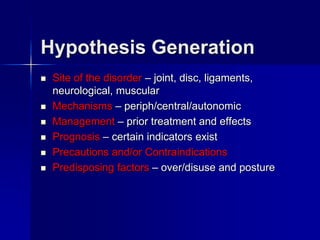
This document provides an overview of the Maitland approach to manual therapy. It defines key terms, outlines the clinical decision making process involving assessment, hypothesis generation and treatment planning. The document describes principles of examining a patient including identifying comparable signs and symptoms, assessing irritability and nature, considering pathology, and designing a treatment plan to address pain or stiffness. The overall summary is that the Maitland approach involves a thorough clinical assessment and examination to develop an individualized treatment plan applying manual therapy techniques.