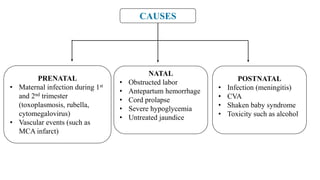
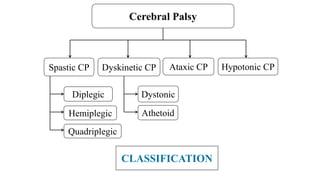
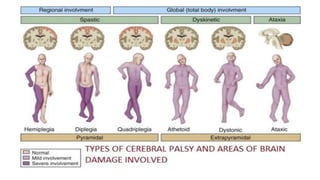
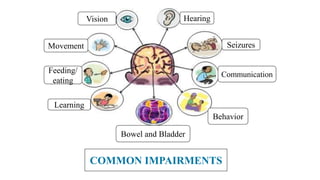
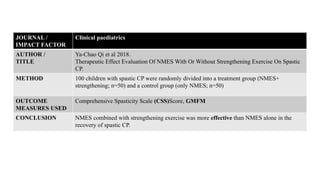
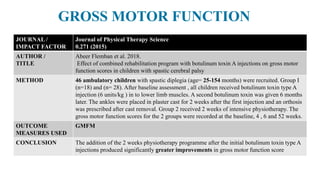
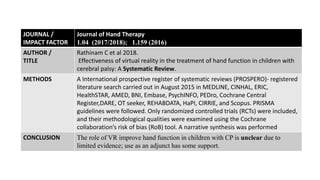
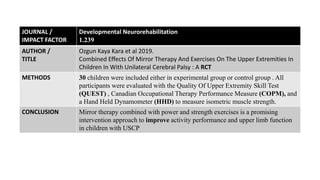
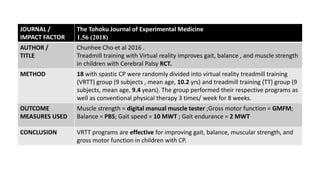
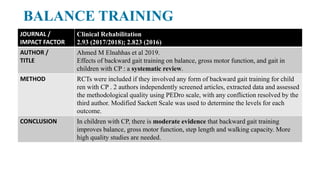
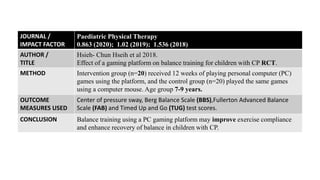
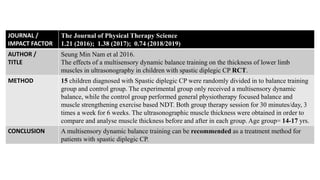
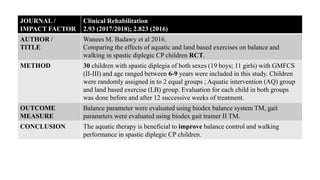
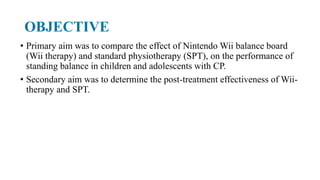
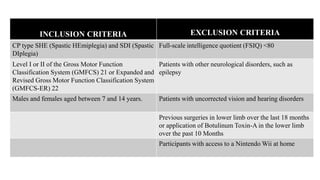
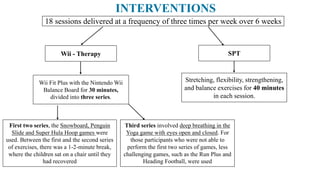
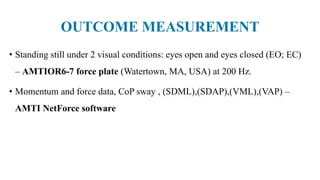
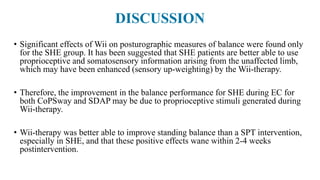
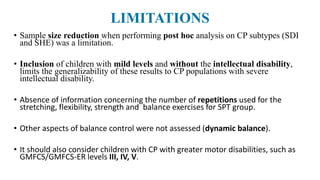
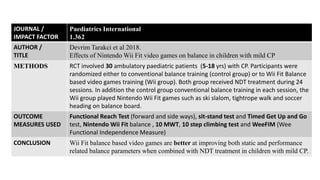
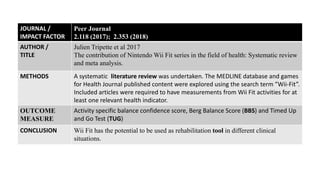
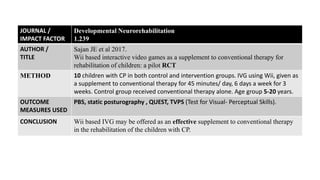
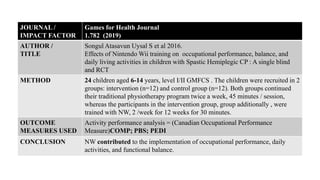
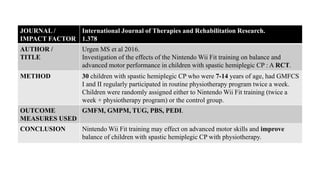
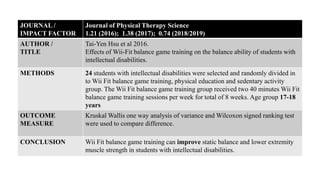
This document provides an overview of interventions to improve balance in children with cerebral palsy. It defines cerebral palsy and discusses its causes, classifications, common impairments, diagnosis and prognosis. It then summarizes several studies on interventions for improving balance, gait, upper extremity function, muscle strength, and postural control in children with cerebral palsy, including stretching, electrical stimulation, virtual reality, treadmill training, mirror therapy, and balance training. The studies examined the effects of these interventions on outcomes like gross motor function, muscle strength, and balance.