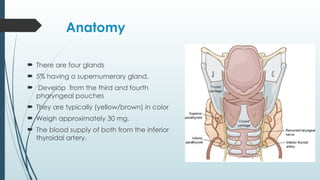
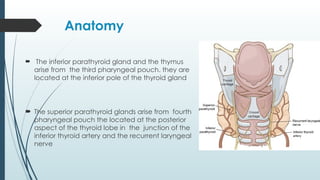
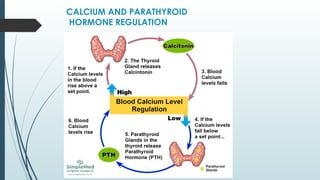
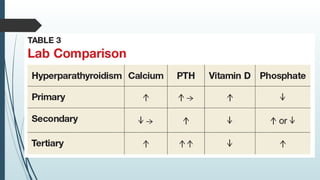
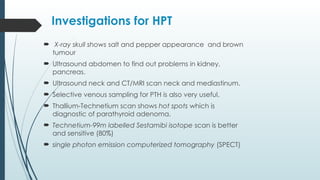
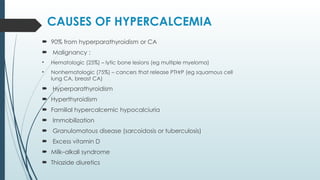
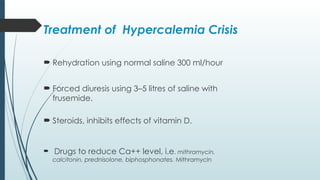
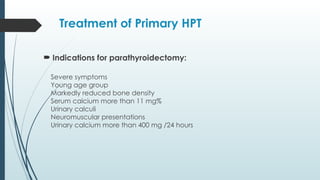
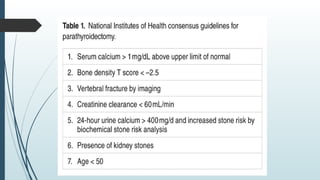
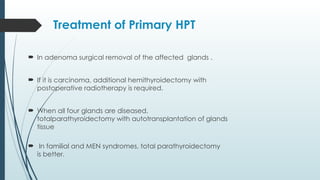
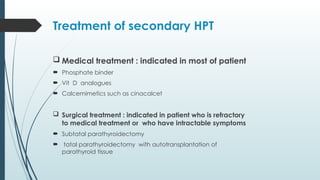
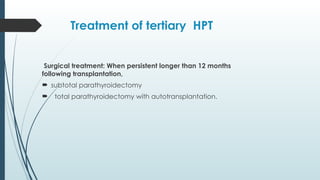
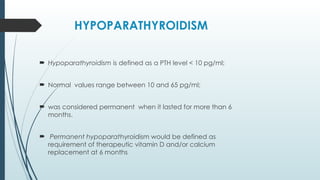
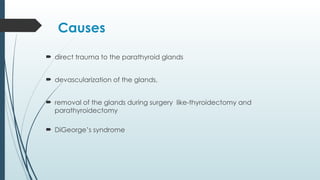
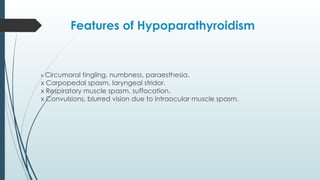
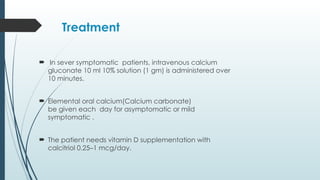
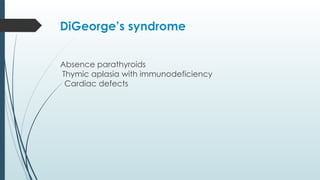
The document provides a comprehensive overview of the anatomy, physiology, and pathophysiology of the parathyroid glands, focusing on conditions such as hyperparathyroidism and hypoparathyroidism. It details the causes, clinical manifestations, diagnostic investigations, and treatment options for these conditions. Additionally, it discusses the implications of related syndromes and surgical considerations in management.