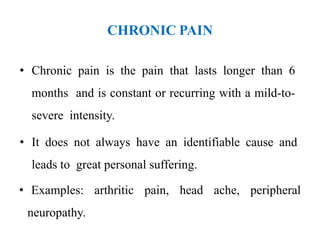
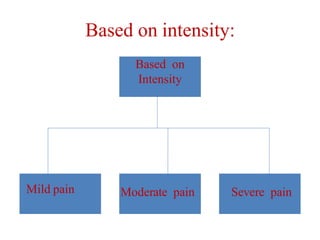
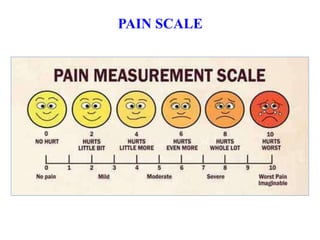
Pain is a complex, subjective experience that can be acute or chronic in nature. It is influenced by physiological, psychological, social, and cultural factors. Pain is assessed using tools like verbal rating scales, numeric rating scales, or the Wong-Baker Faces scale. Both pharmacological and non-pharmacological methods are used for pain management, with pharmacological methods including non-opioid analgesics, opioid analgesics, and adjuvant medications according to the WHO pain ladder. Patient-controlled analgesia allows patients more control over their pain medication delivery.