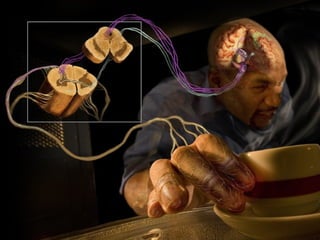
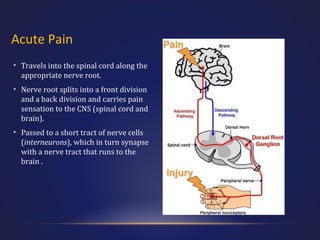
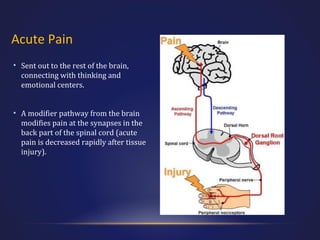
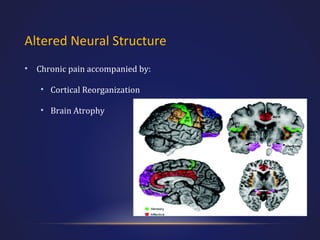
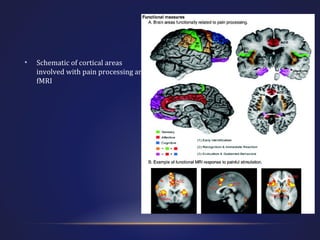
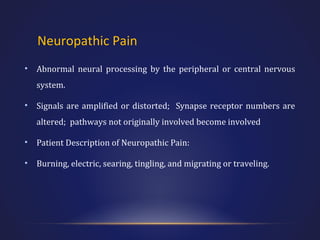
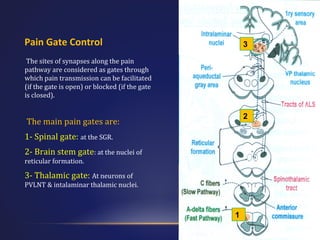
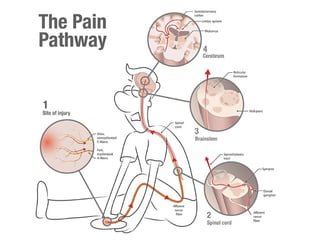
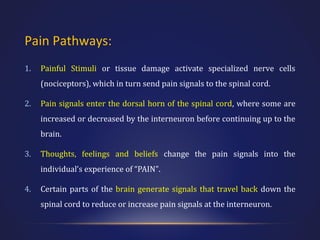
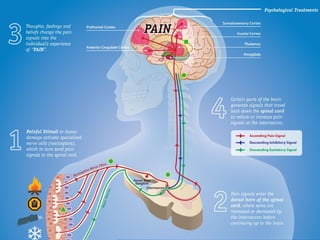
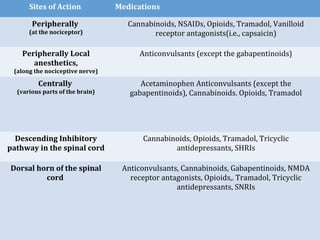
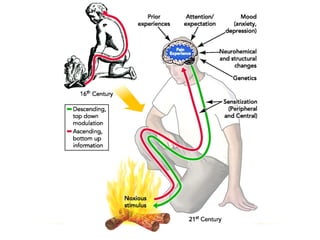
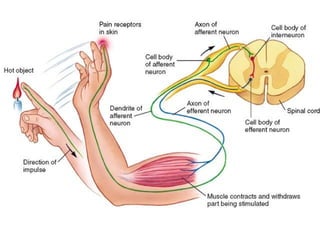
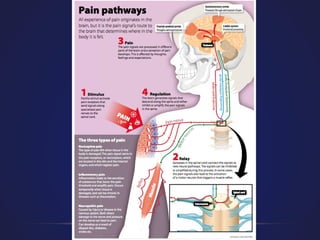
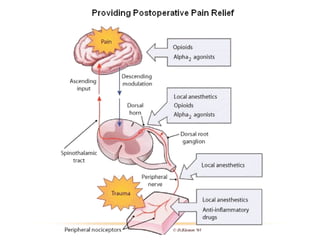
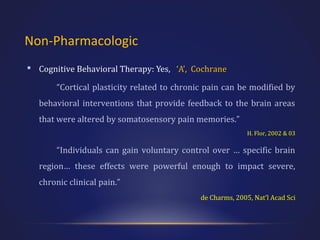
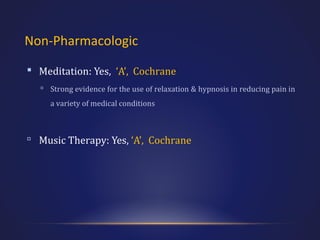
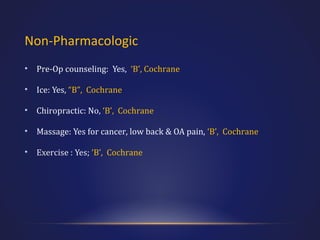
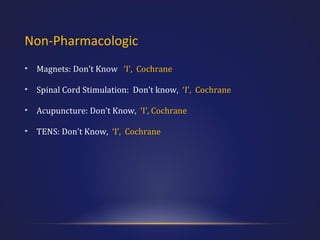
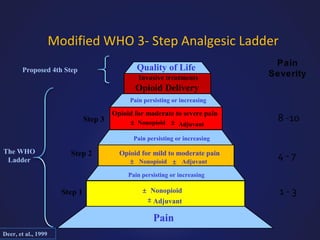
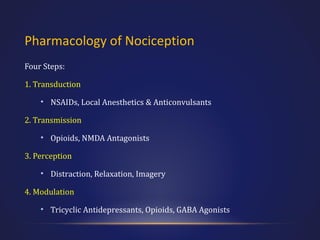
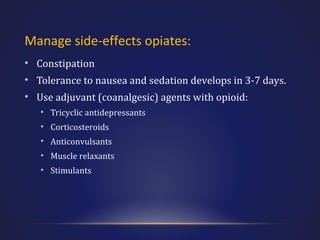
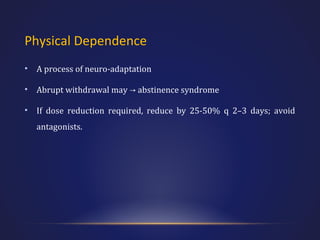
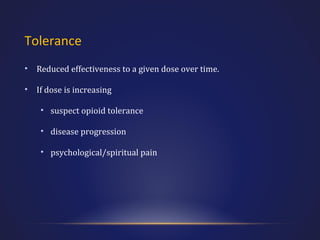
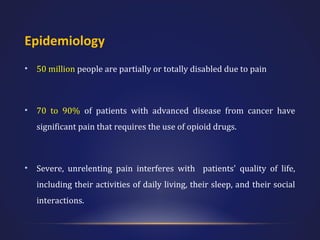
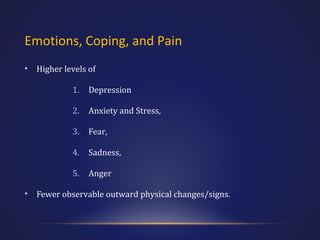
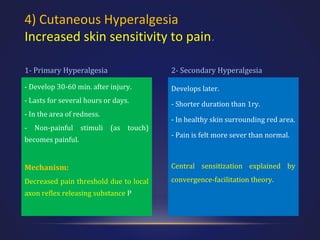
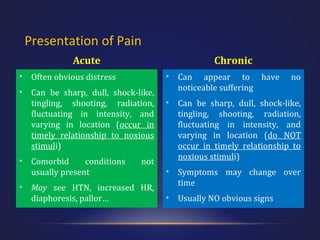
This document provides an overview of pain medicine. It defines pain and discusses its epidemiology, economics, and physiological effects. It describes acute and chronic pain, including their presentations and pathophysiology. Neuropathic and nociceptive pain are major categories discussed. Pain pathways and the gate control theory of pain are also summarized. Psychiatric comorbidities with chronic pain are noted.




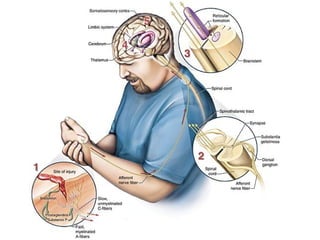
![Acute Pain (Nociceptive)
• Somatic
• Superficial (nociceptors of skin)
• Deep [body wall (muscle, bone)]
• Visceral (sympathetic system; may refer to
superficial structures of same spinal nerve)](https://image.slidesharecdn.com/drsafaripainmanagement-131129111404-phpapp01/85/Pain-Management-General-concepts-and-primary-discussions-30-320.jpg)