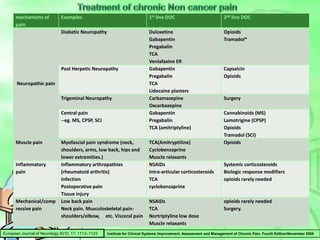
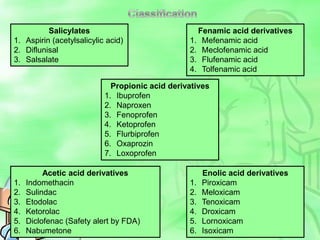
This document discusses pain and its treatment. It begins by defining pain and classifying common types of pain conditions. It then discusses the body's reflex responses to pain and the endorphin system that modulates pain. It describes the differences between acute and chronic pain and methods of pain measurement. Various treatment options are provided for different types of pain, including NSAIDs, opioids, tramadol, tapentadol, muscle relaxants, and sodium channel blockers. Newer treatments discussed include epirisone and the comparative properties of different NSAIDs, muscle relaxants, tramadol, and tapentadol. Key questions are also provided about comparing treatment effectiveness and safety across patient subgroups.






















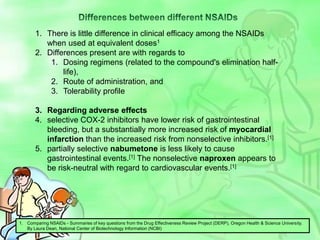











![Differences between different NSAIDsThere is little difference in clinical efficacy among the NSAIDs when used at equivalent doses1Differences present are with regards to Dosing regimens (related to the compound's elimination half-life), Route of administration, and Tolerability profileRegarding adverse effectsselective COX-2 inhibitors have lower risk of gastrointestinal bleeding, but a substantially more increased risk of myocardial infarction than the increased risk from nonselective inhibitors.[1]partially selective nabumetone is less likely to cause gastrointestinal events.[1] The nonselective naproxen appears to be risk-neutral with regard to cardiovascular events.[1]Comparing NSAIDs - Summaries of key questions from the Drug Effectiveness Review Project (DERP), Oregon Health & Science University. By Laura Dean, National Center of Biotechnology Information (NCBI)](https://image.slidesharecdn.com/pain-110921104554-phpapp01/85/Pain-Management-Current-Newer-Modalities-37-320.jpg)












