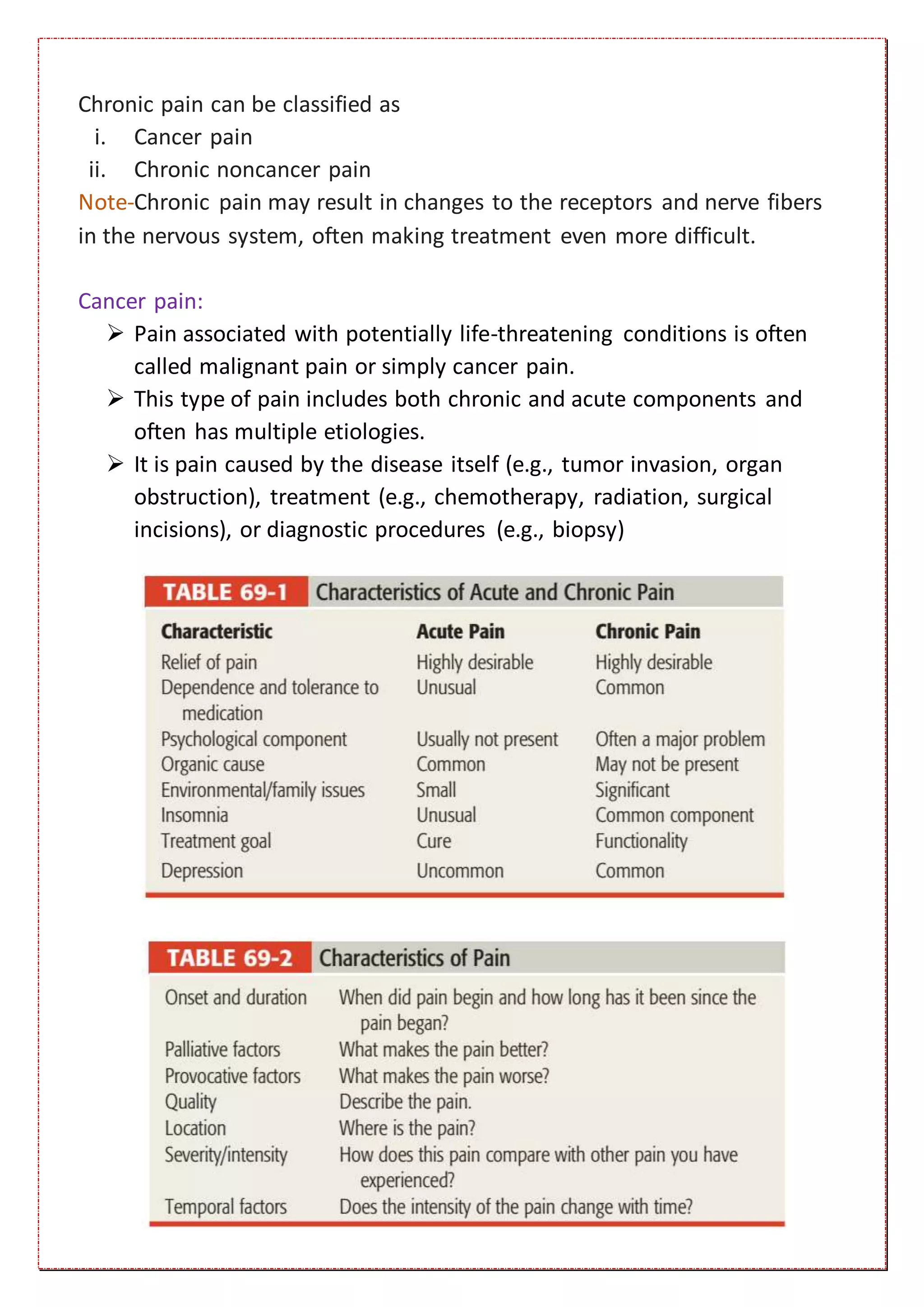
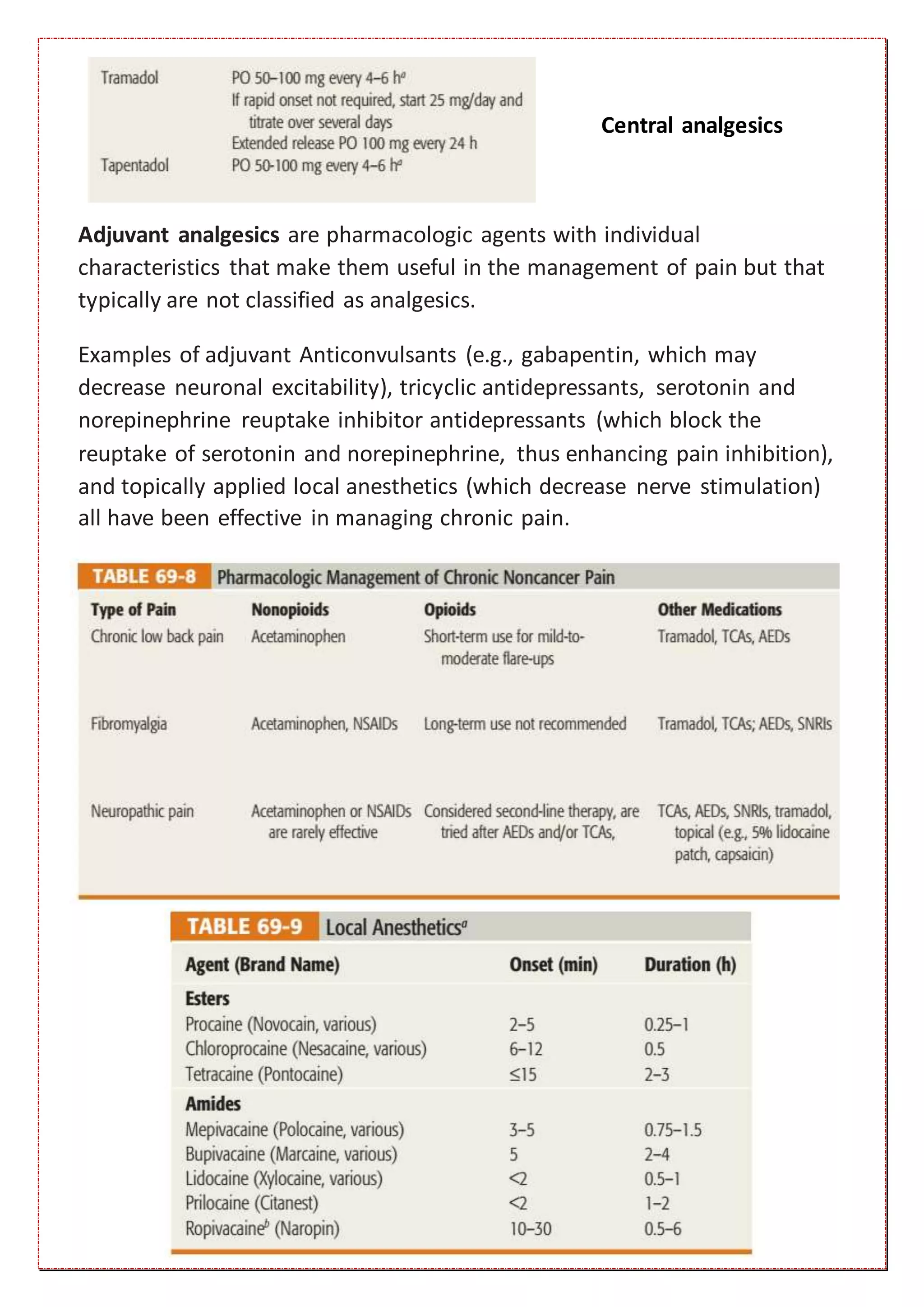
Pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage. There are two main types of pain: nociceptive pain which arises from skin, bone, joint, muscle or connective tissue and visceral pain which arises from internal organs. Neuropathic pain arises from damage or dysfunction of the nervous system. Acute pain serves a protective purpose but can become chronic pain lasting months to years. Chronic pain is more difficult to treat and often involves comorbid conditions like insomnia or depression. Pain is diagnosed based on patient history and description as there are no specific tests. Treatment involves both nonpharmacological options like heat/cold therapy and exercise as well as pharmacological options like nonopioid analgesics, opioid