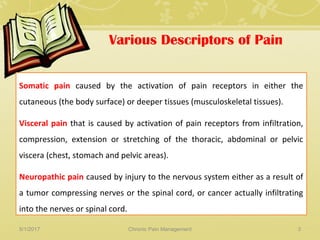
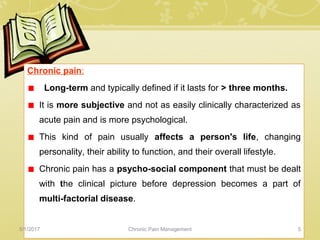
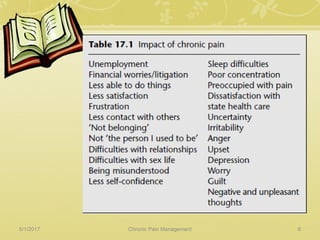
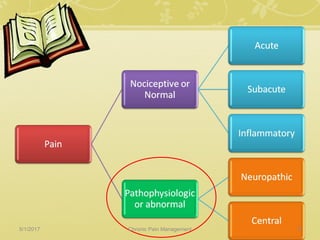
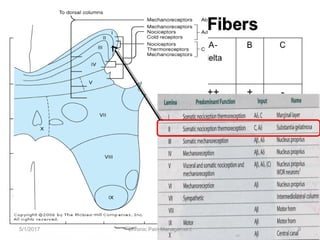
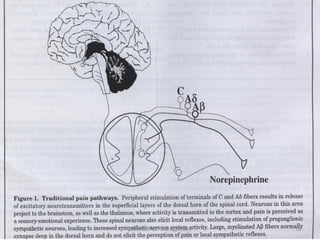
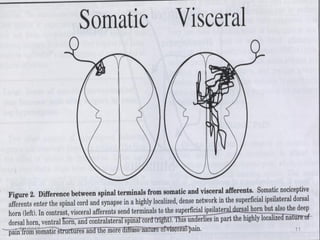
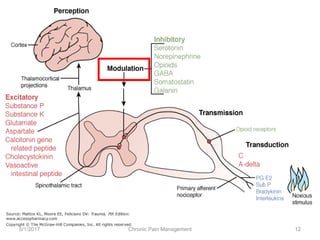
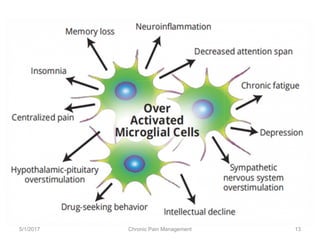
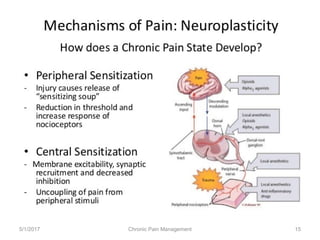
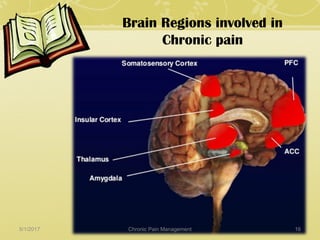
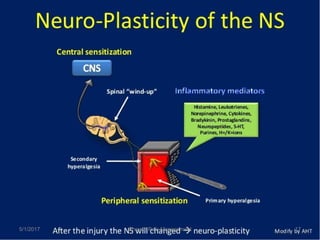
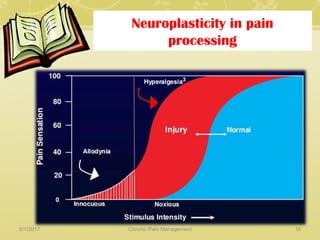
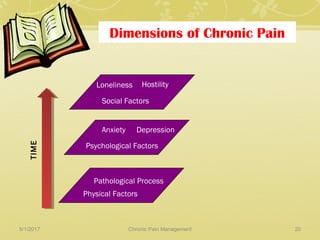
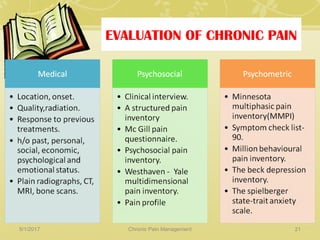
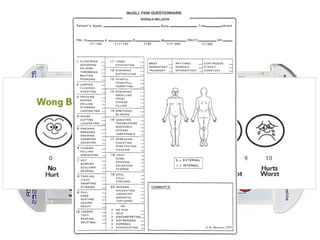
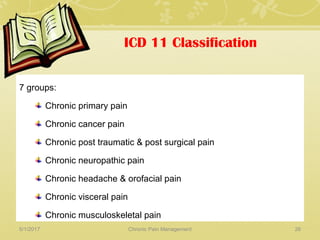
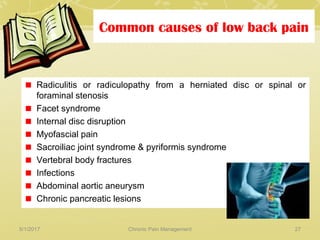
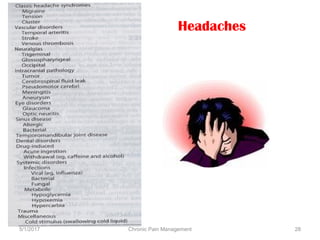
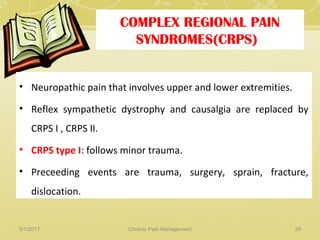
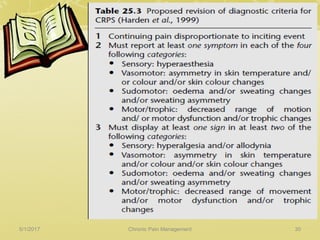
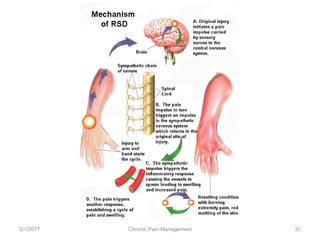
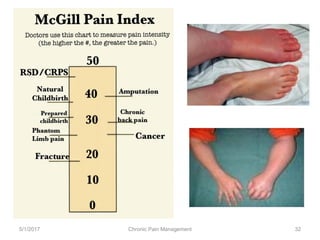
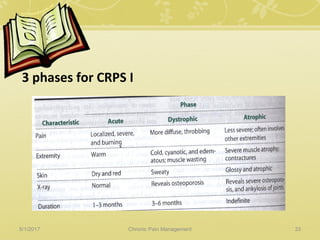
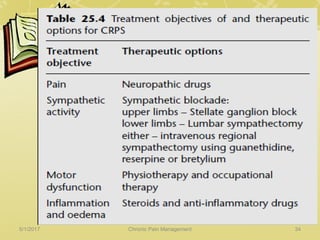
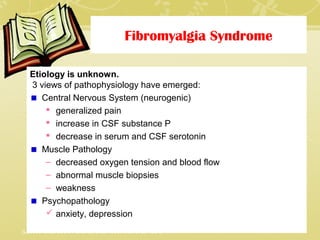
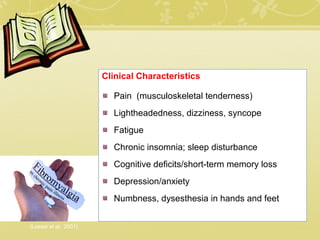
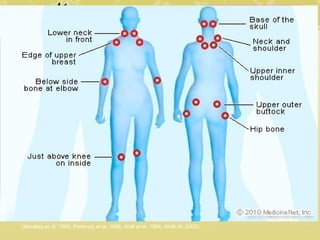
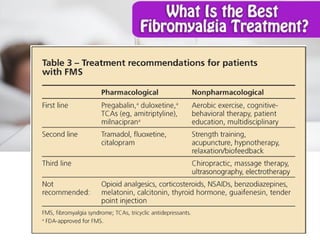
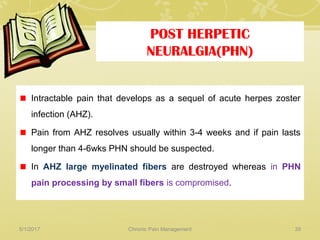
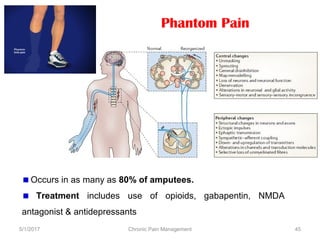
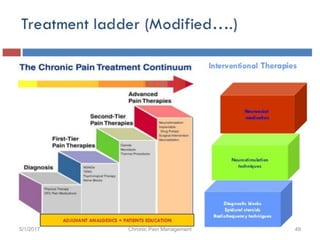
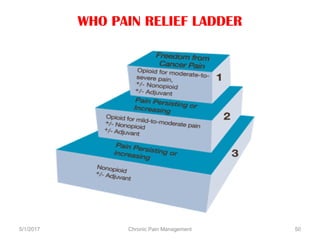
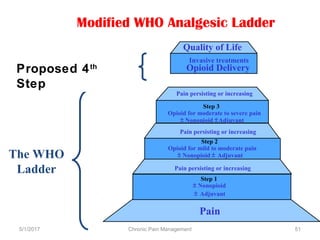
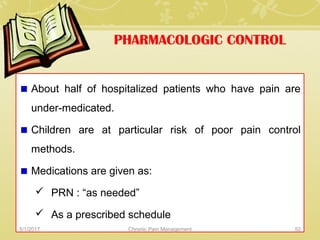
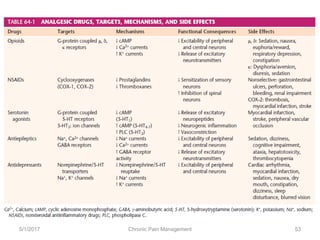
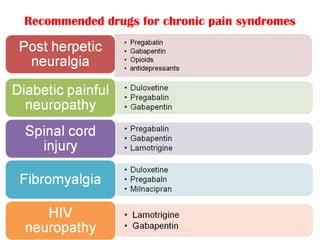
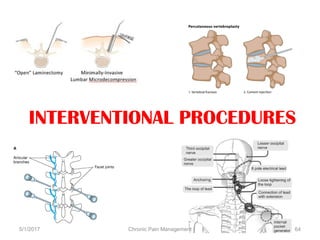
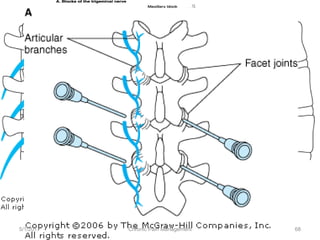
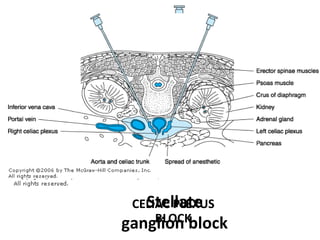
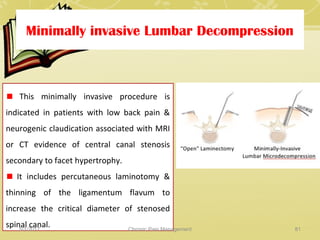
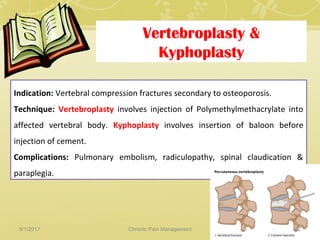
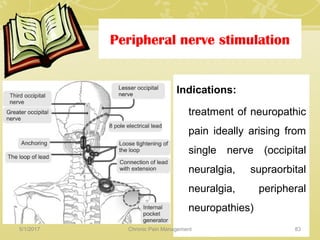
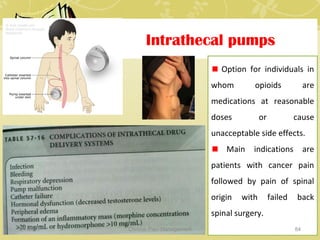
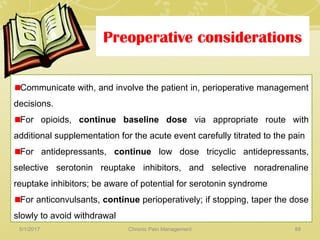
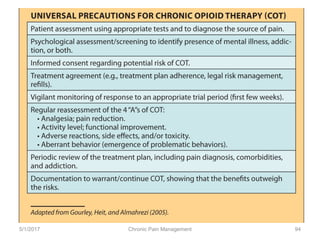
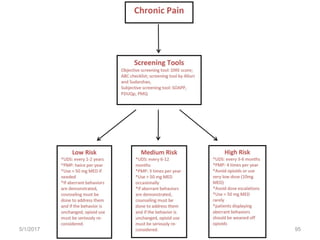
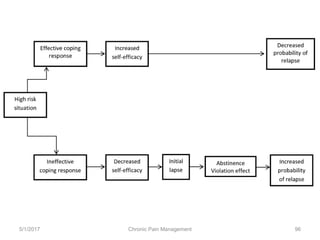
This document discusses chronic pain management. It defines chronic pain as pain lasting over 3 months. It describes different types of pain such as somatic, visceral and neuropathic pain. It discusses various chronic pain conditions like fibromyalgia, complex regional pain syndrome, postherpetic neuralgia and diabetic neuropathy. It covers evaluation of chronic pain, pathophysiology of chronic pain, brain regions involved, and the multidimensional nature of chronic pain including physical, psychological and social factors. Finally, it discusses various management approaches for chronic pain including pharmacological, physical, psychological and invasive techniques.