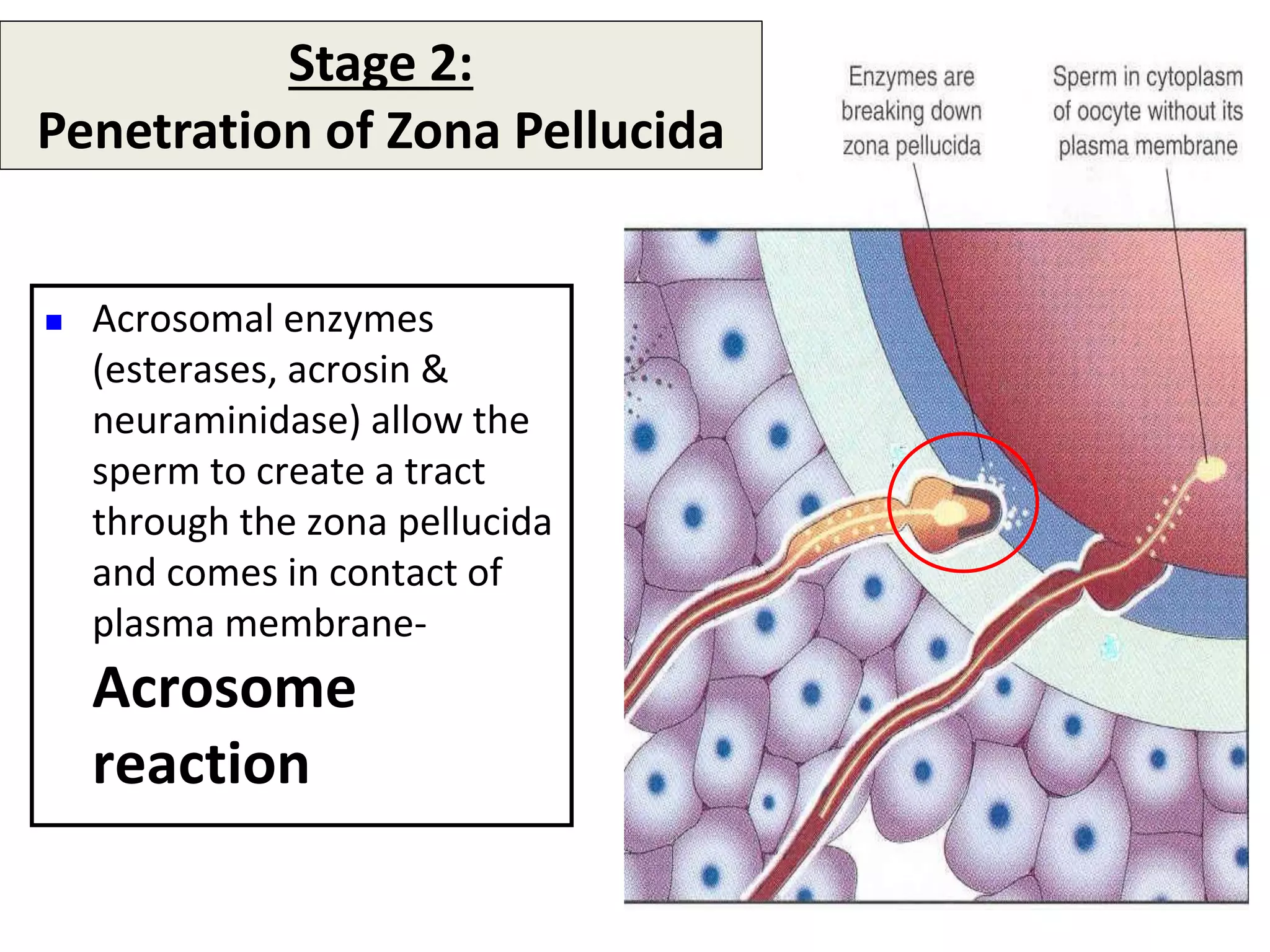
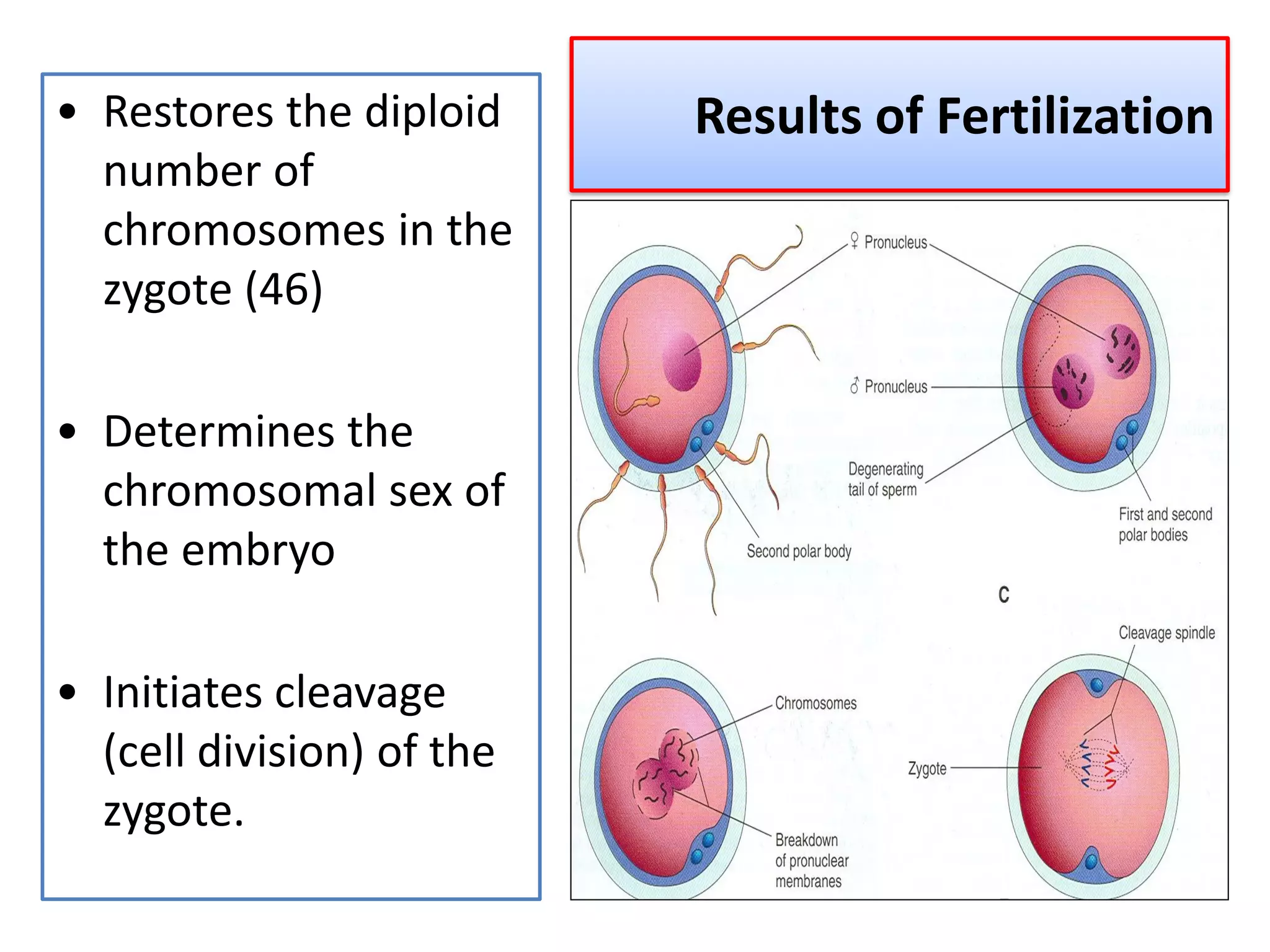
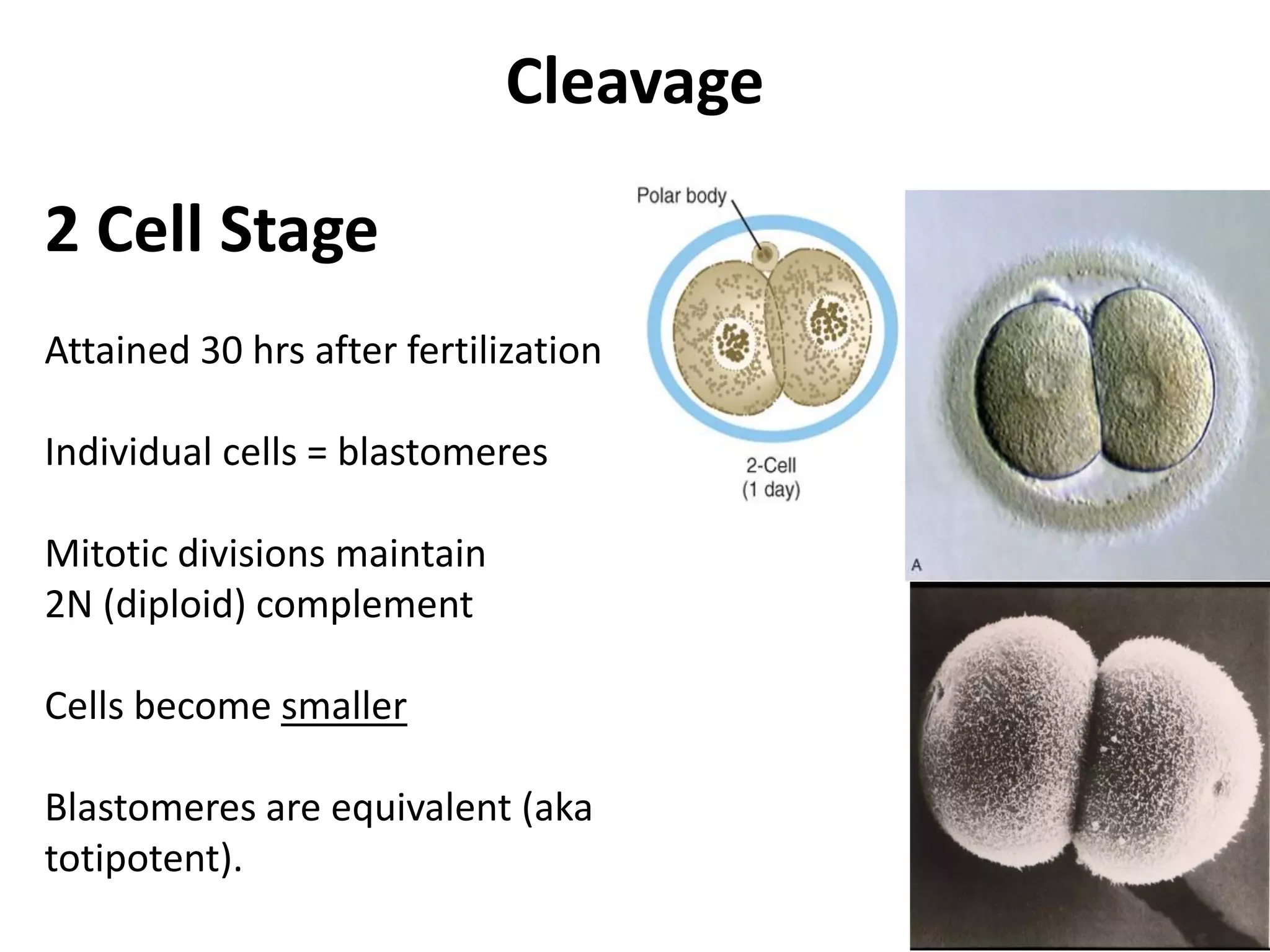
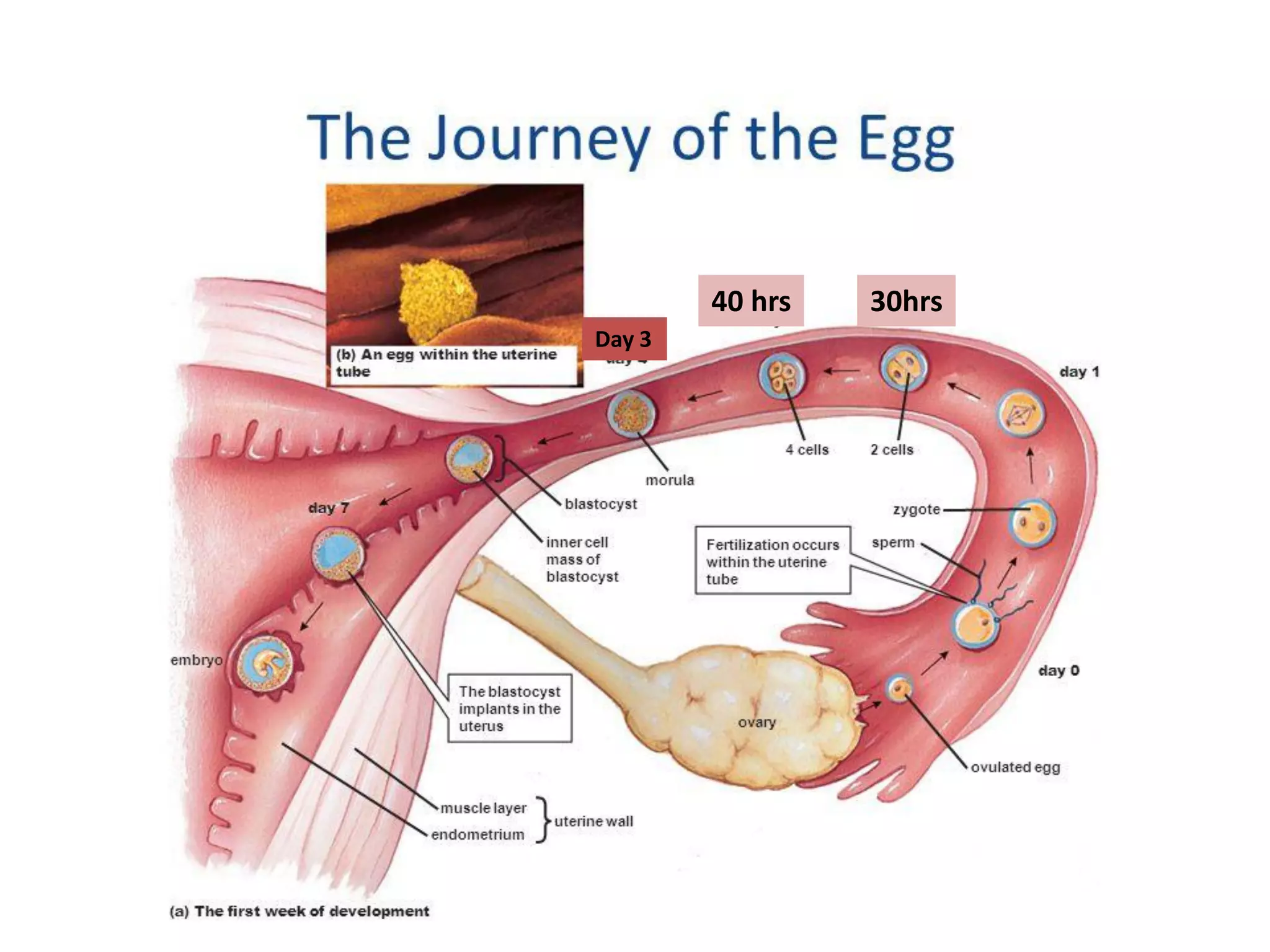
1) Fertilization occurs when a sperm fuses with an egg in the fallopian tube. This initiates cell division and the development of an embryo.
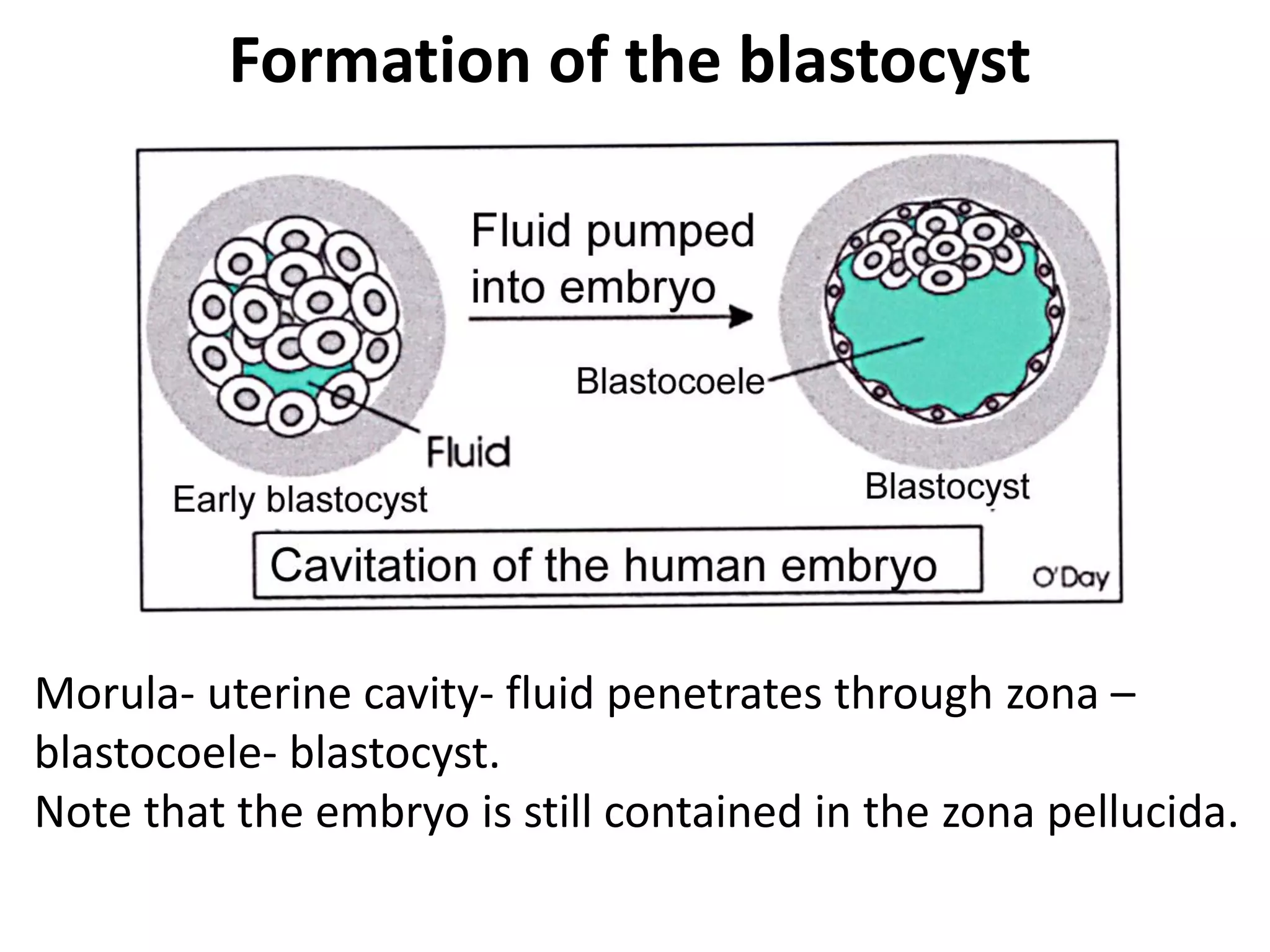
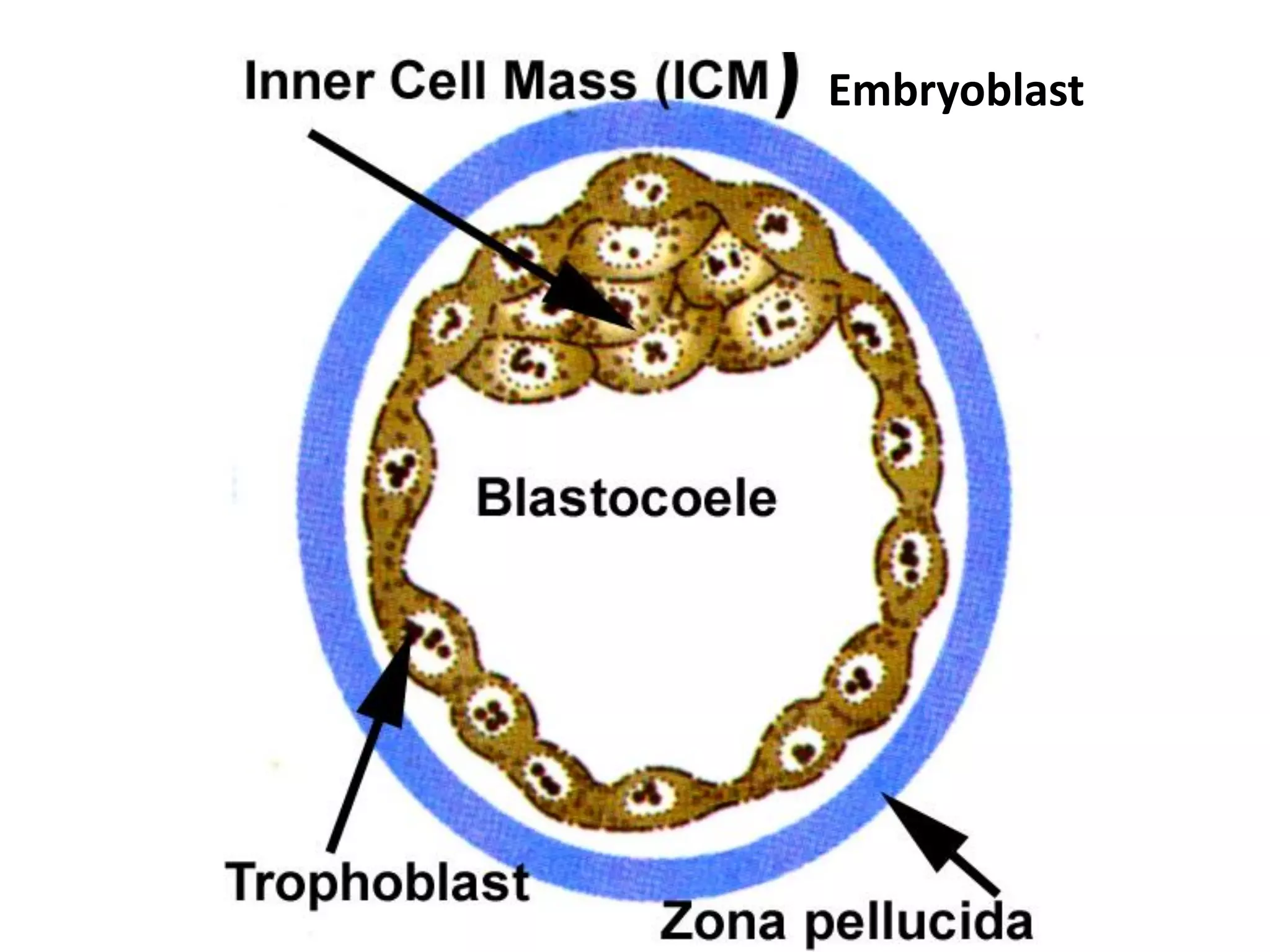
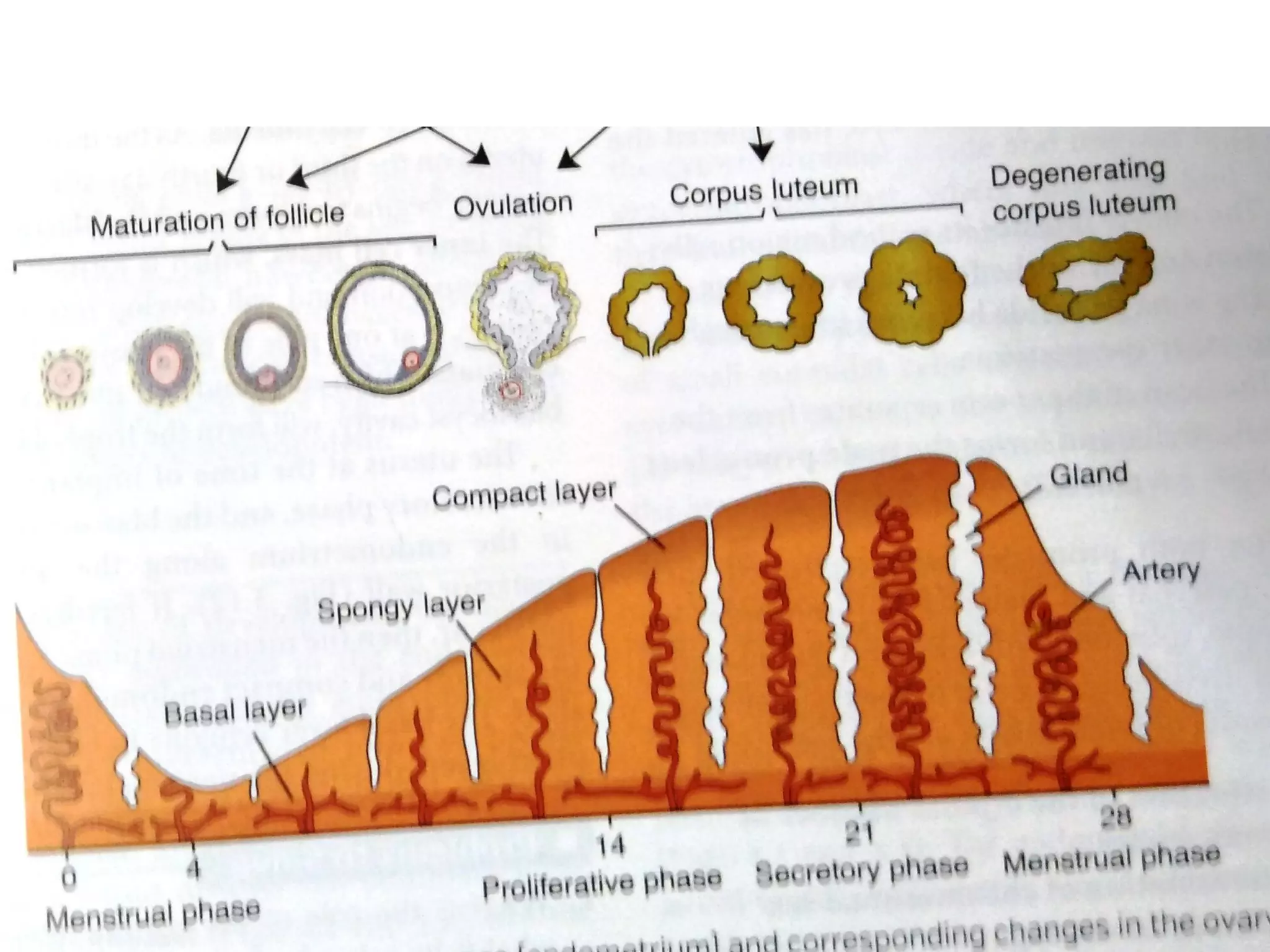
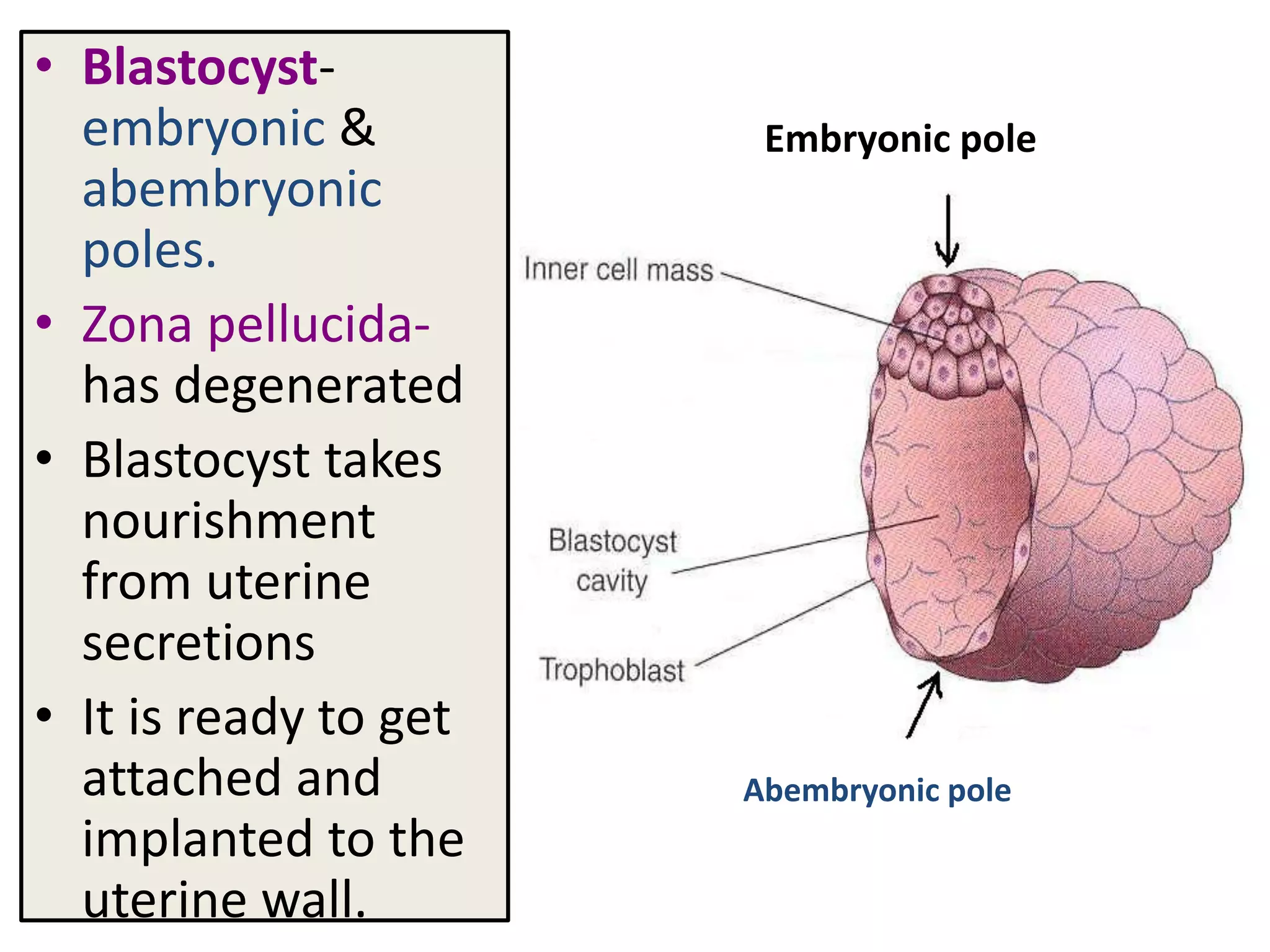
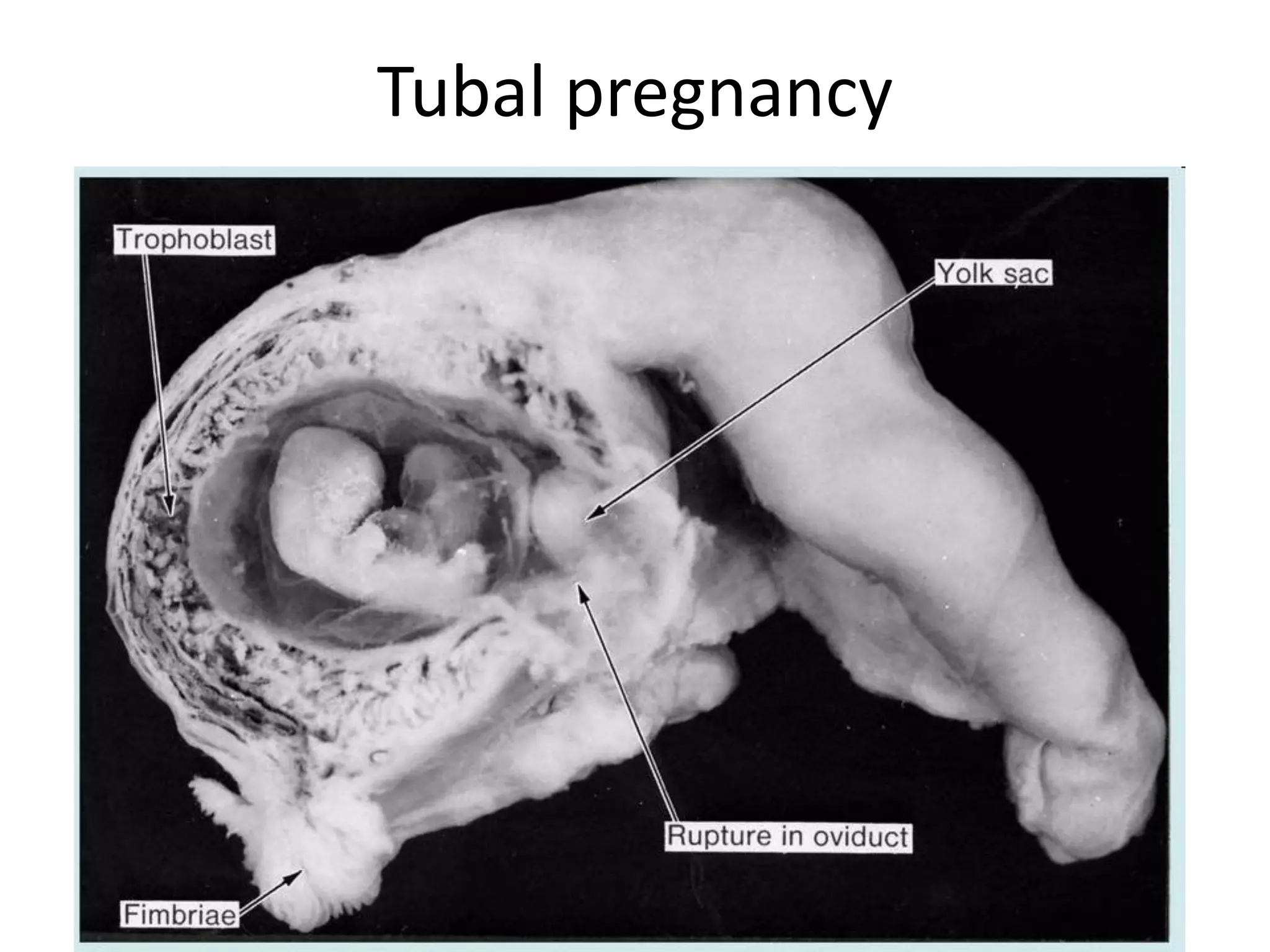
2) By day 5, the embryo has developed into a blastocyst stage and begins to implant in the uterine wall. Implantation is completed by day 12.
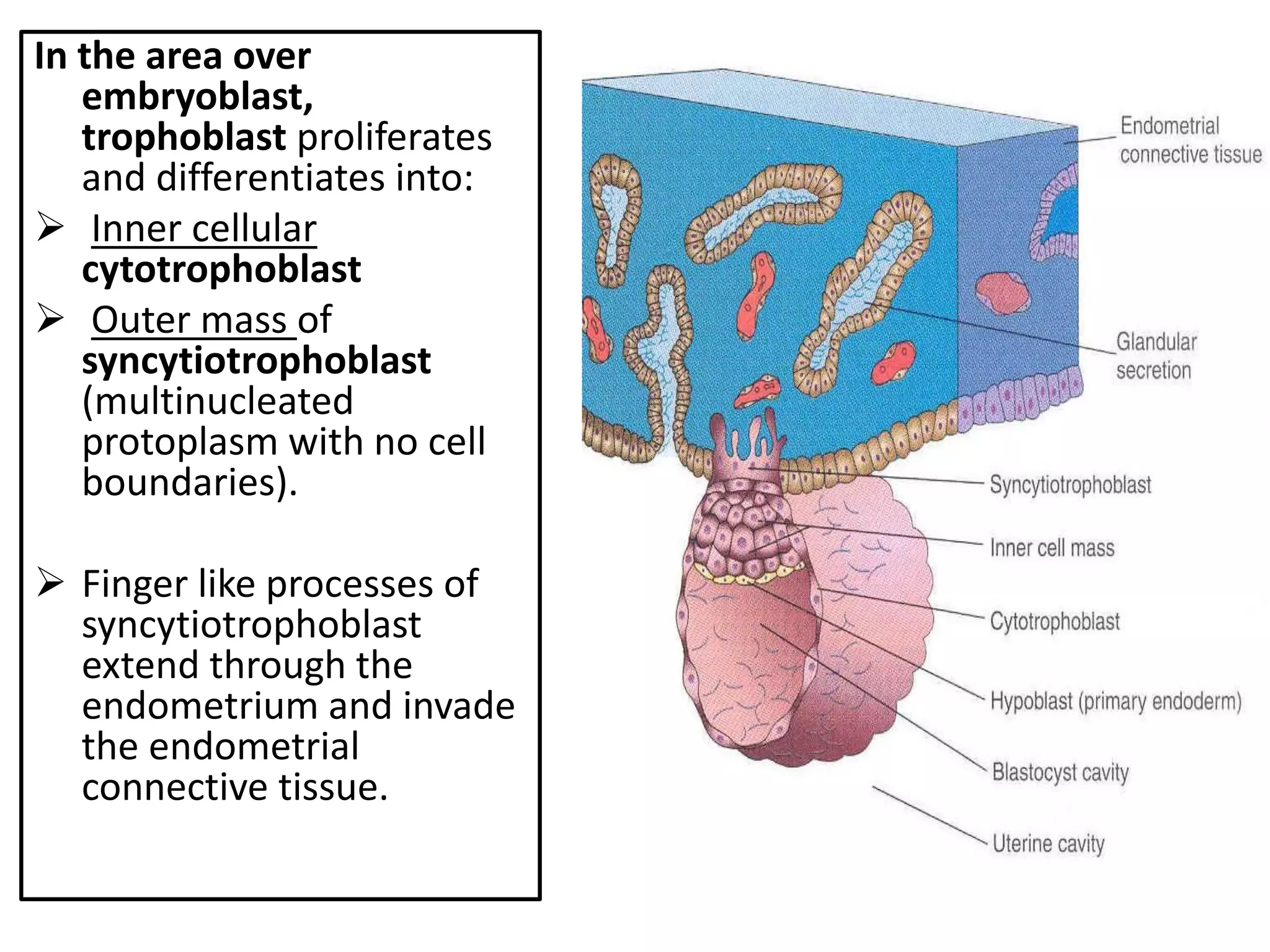
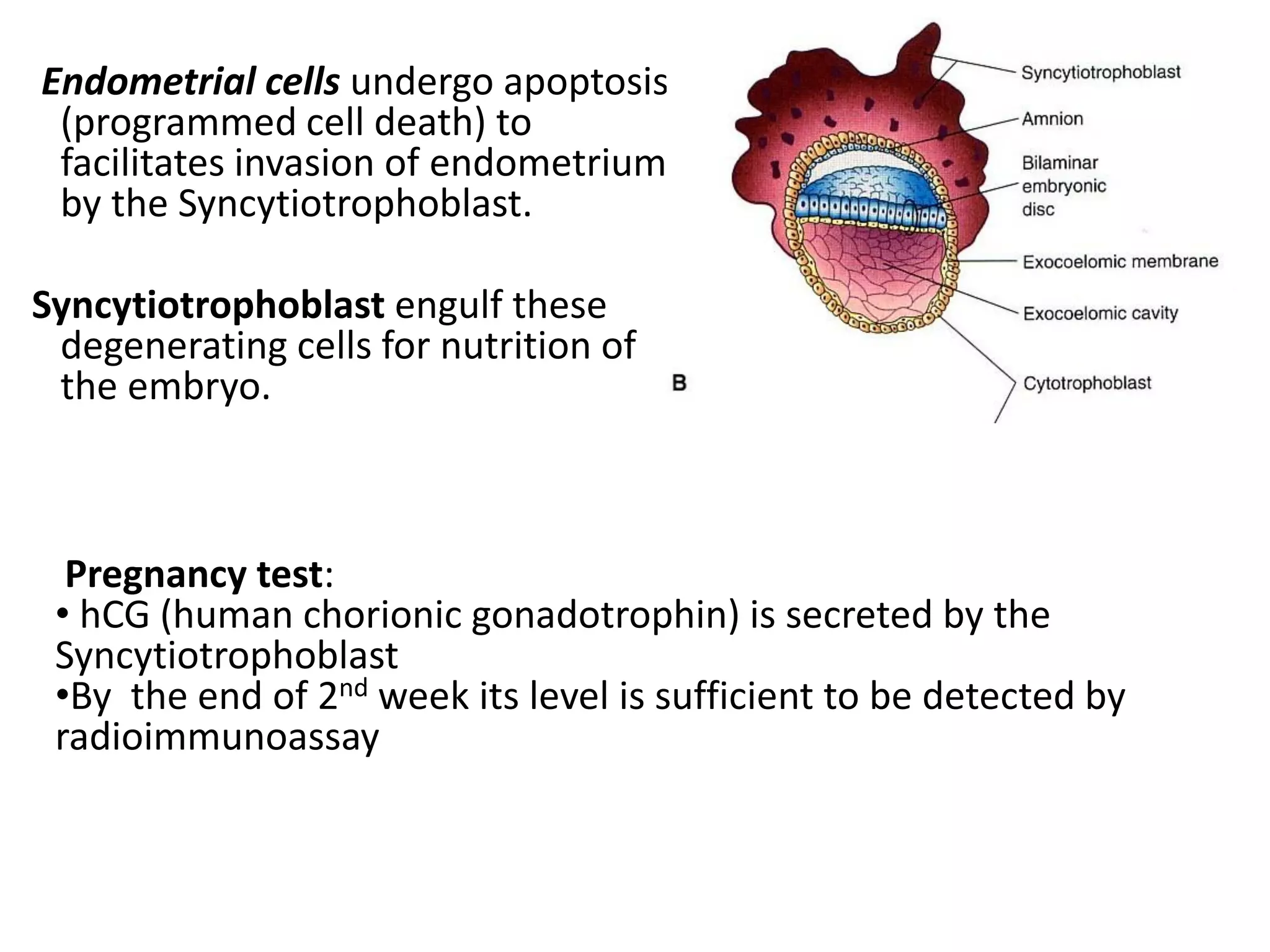
3) For successful implantation, the blastocyst must attach to the endometrium and the trophoblast cells must invade the uterine tissues to establish blood flow from the mother. This allows the embryo to receive nutrients for growth and development of a pregnancy.