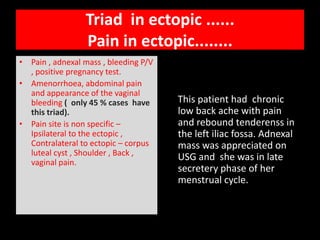
The document discusses the diagnosis and management of ovarian ectopic pregnancy, detailing a case of a 27-year-old female with symptoms and imaging findings indicative of this condition. It highlights the importance of differentiating between ectopic pregnancies and other ovarian and pelvic masses, especially using ultrasound and beta HCG levels. The text also elaborates on the diagnostic criteria for ectopic pregnancies, current treatment options, and factors influencing the detection and management of these cases.