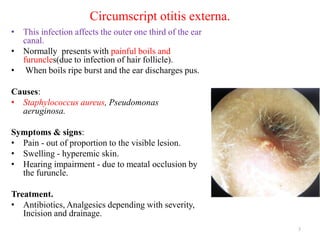
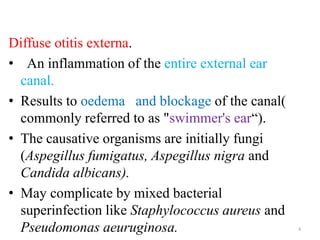
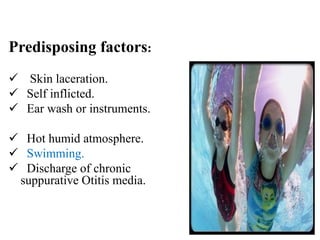
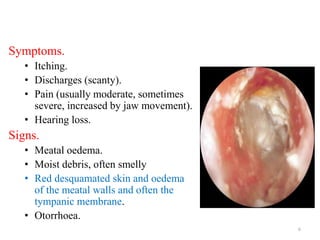
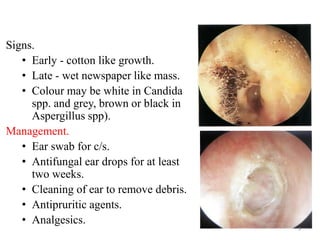
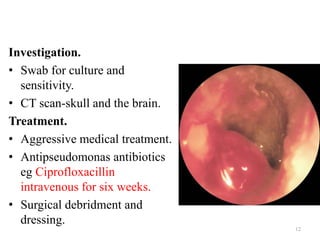
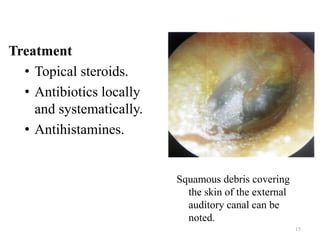
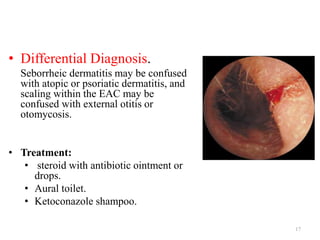
Otitis externa encompasses various inflammatory conditions of the external auditory meatus, classified into infectious, reactive, and seborrheic types. Symptoms include pain, swelling, hearing impairment, and in severe cases, necrotizing infections affecting the skull bases and cranial nerves. Treatment varies based on the type and severity of infection, often involving antibiotics, antifungals, and surgical intervention for complications.