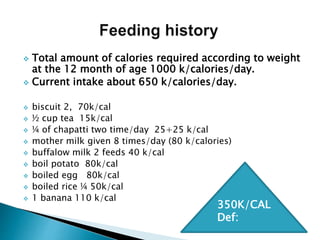
A 12-month-old female child was admitted with fever, cough, and shortness of breath. Her history included recurrent pneumonia. On examination, she had respiratory distress, hepatosplenomegaly, and low weight. Tests found elevated lipids and bone marrow cells resembling Niemann-Pick cells. The child was suspected of having Niemann-Pick Disease type B, a rare genetic disorder caused by a lipid metabolism enzyme deficiency. Type B presents in infancy with lung and liver involvement. No specific treatment exists but management focuses on supportive care.