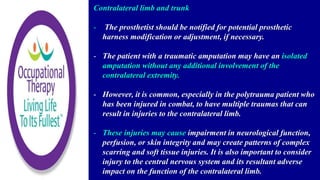
1. An amputation care team should take an interdisciplinary approach to managing patients with upper extremity amputations. This includes regular communication to develop a comprehensive treatment plan.
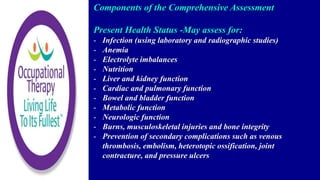
2. Comprehensive assessments should be completed during the perioperative, pre-prosthetic, and prosthetic training phases, as well as annual screenings, to document outcomes and monitor rehabilitation efficacy.
3. Rehabilitation should have a patient-centered approach, incorporating patient goals and providing education, from the perioperative phase through lifelong care.