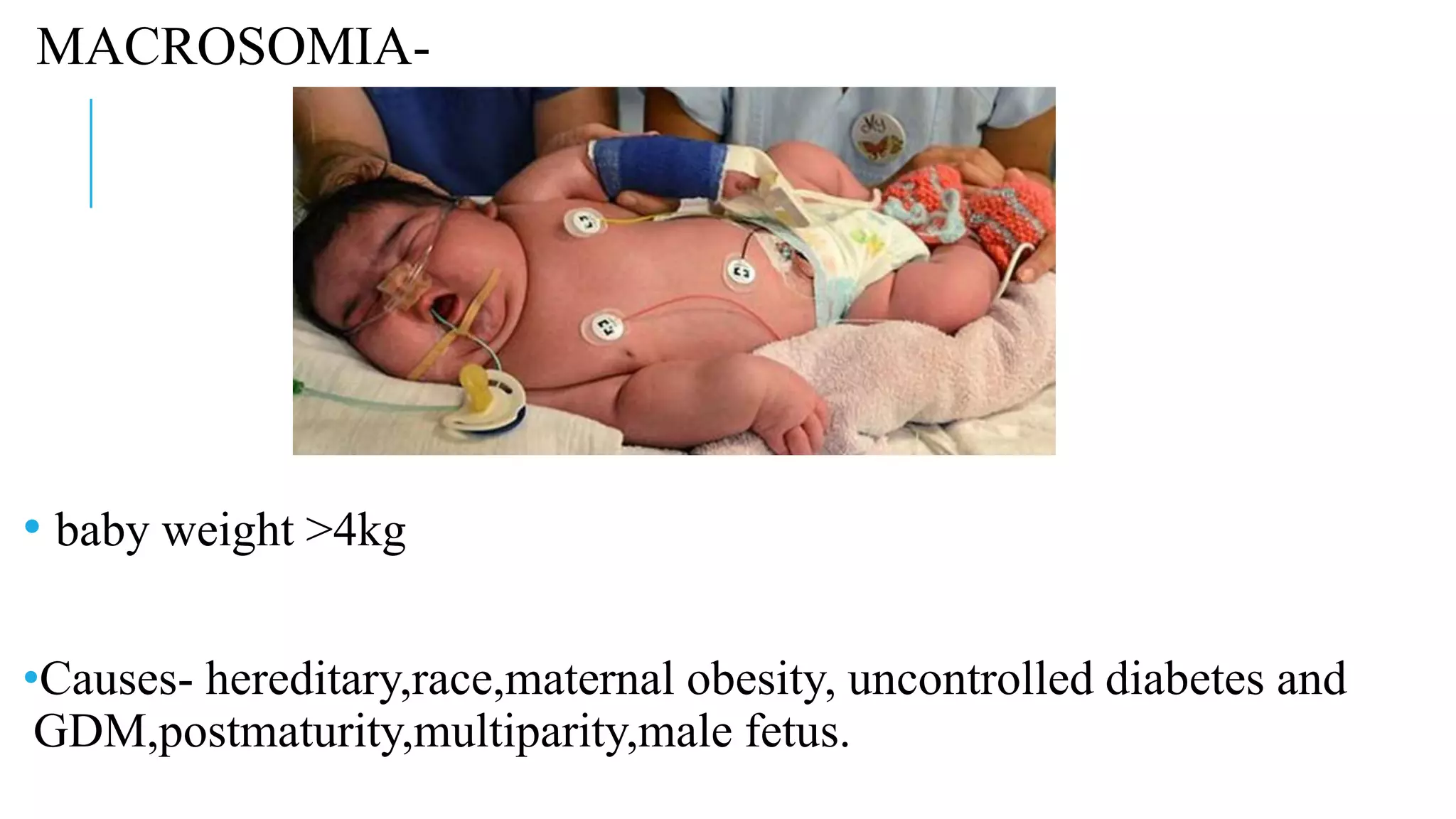
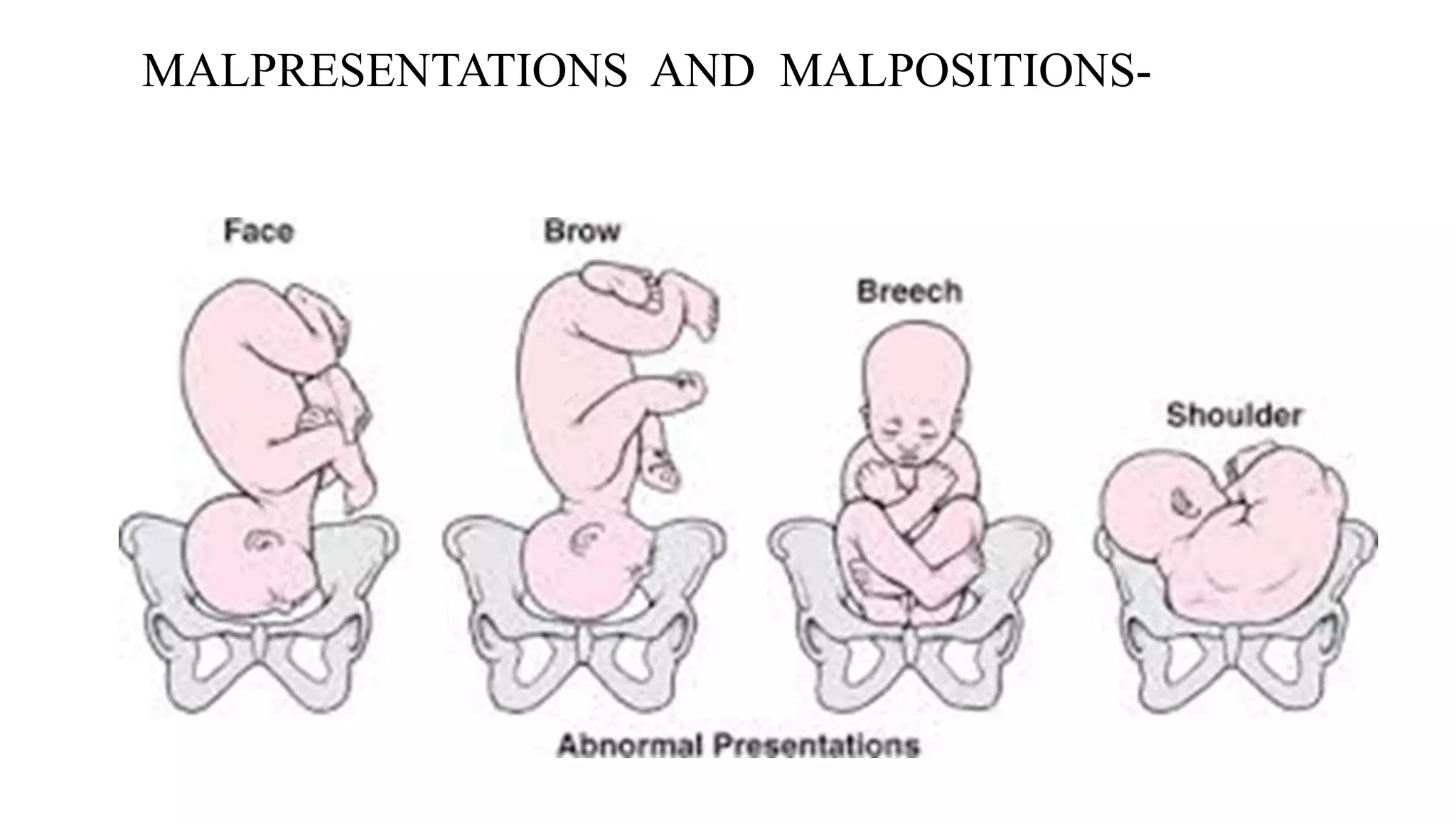
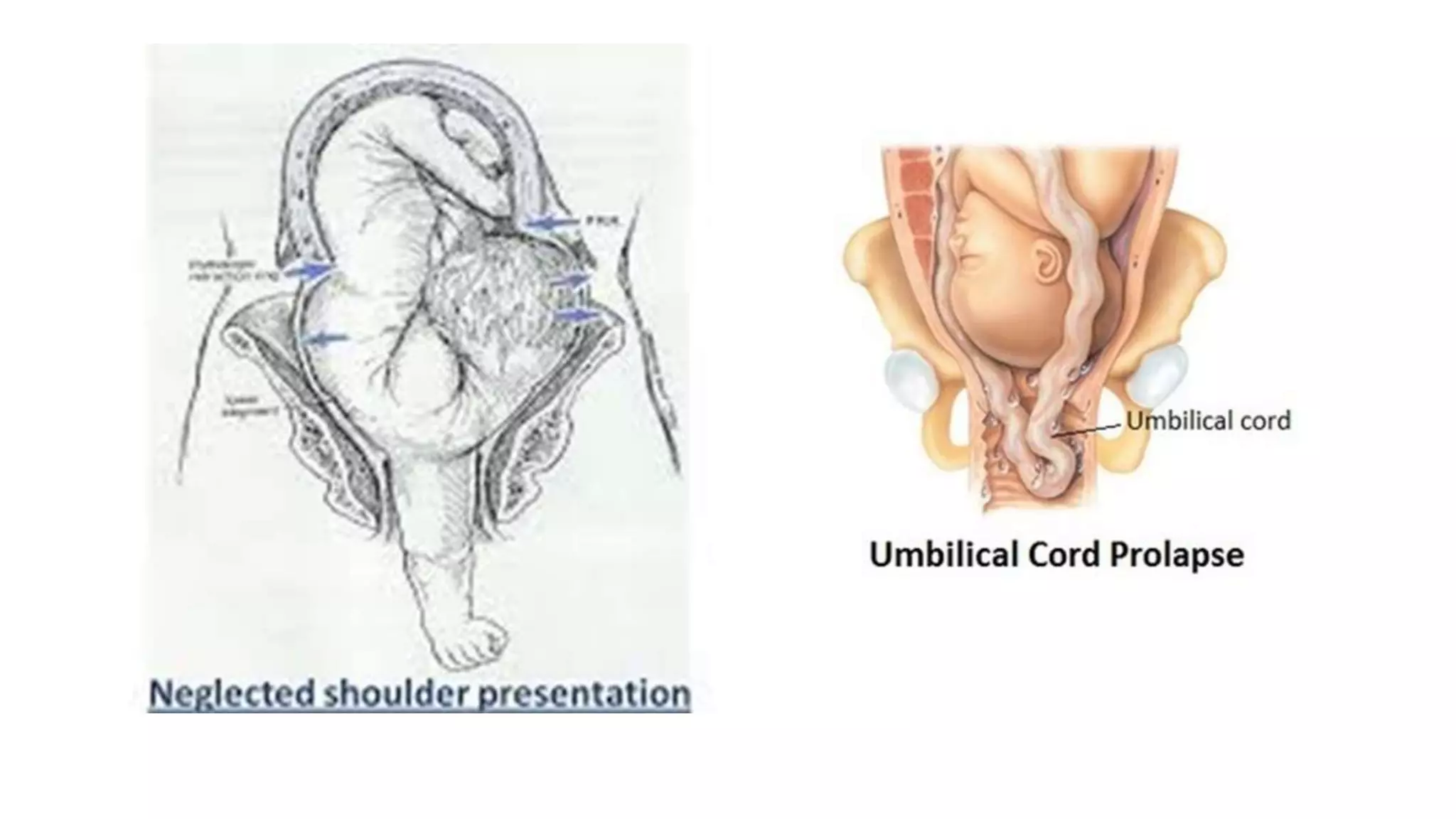
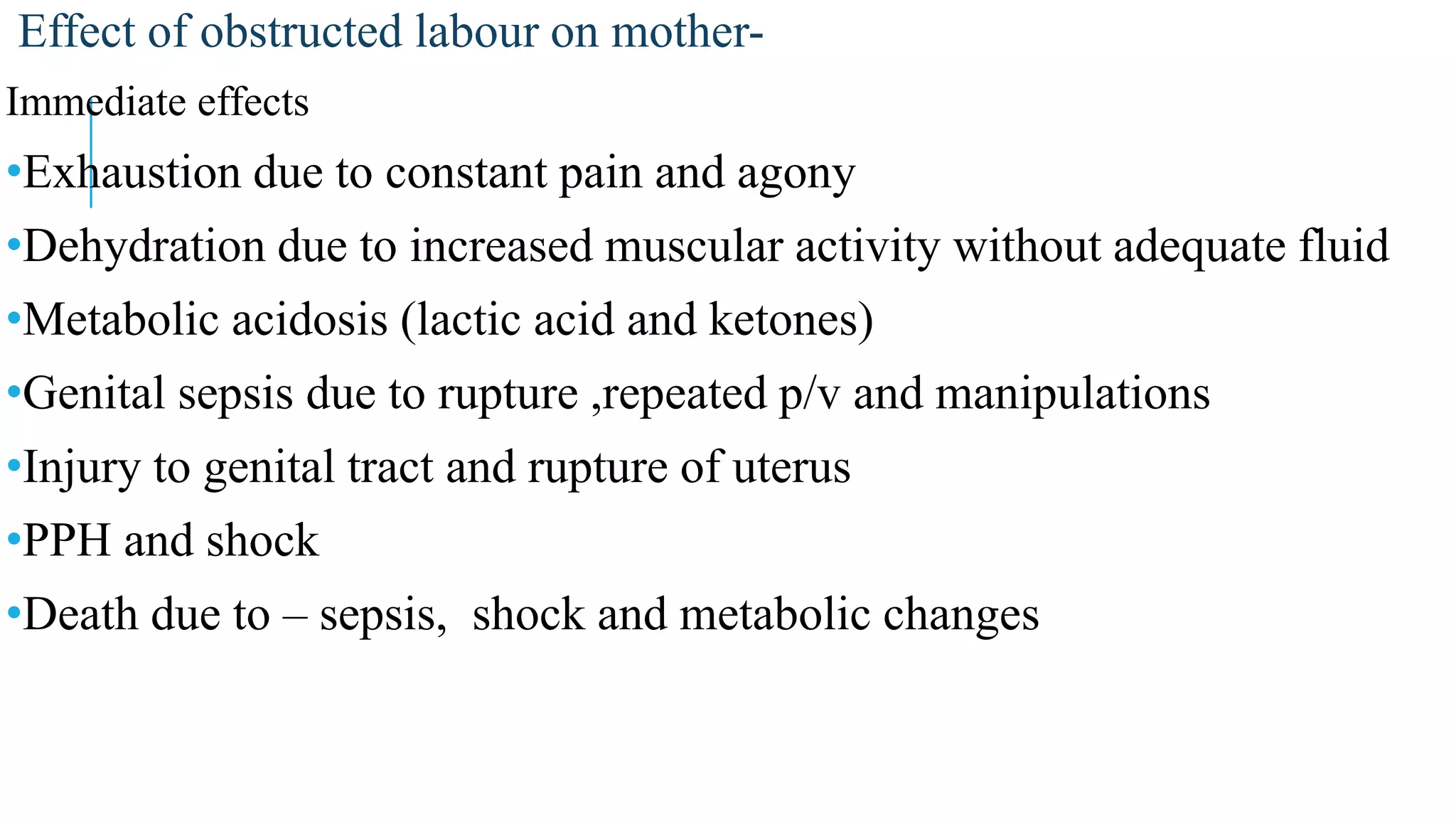
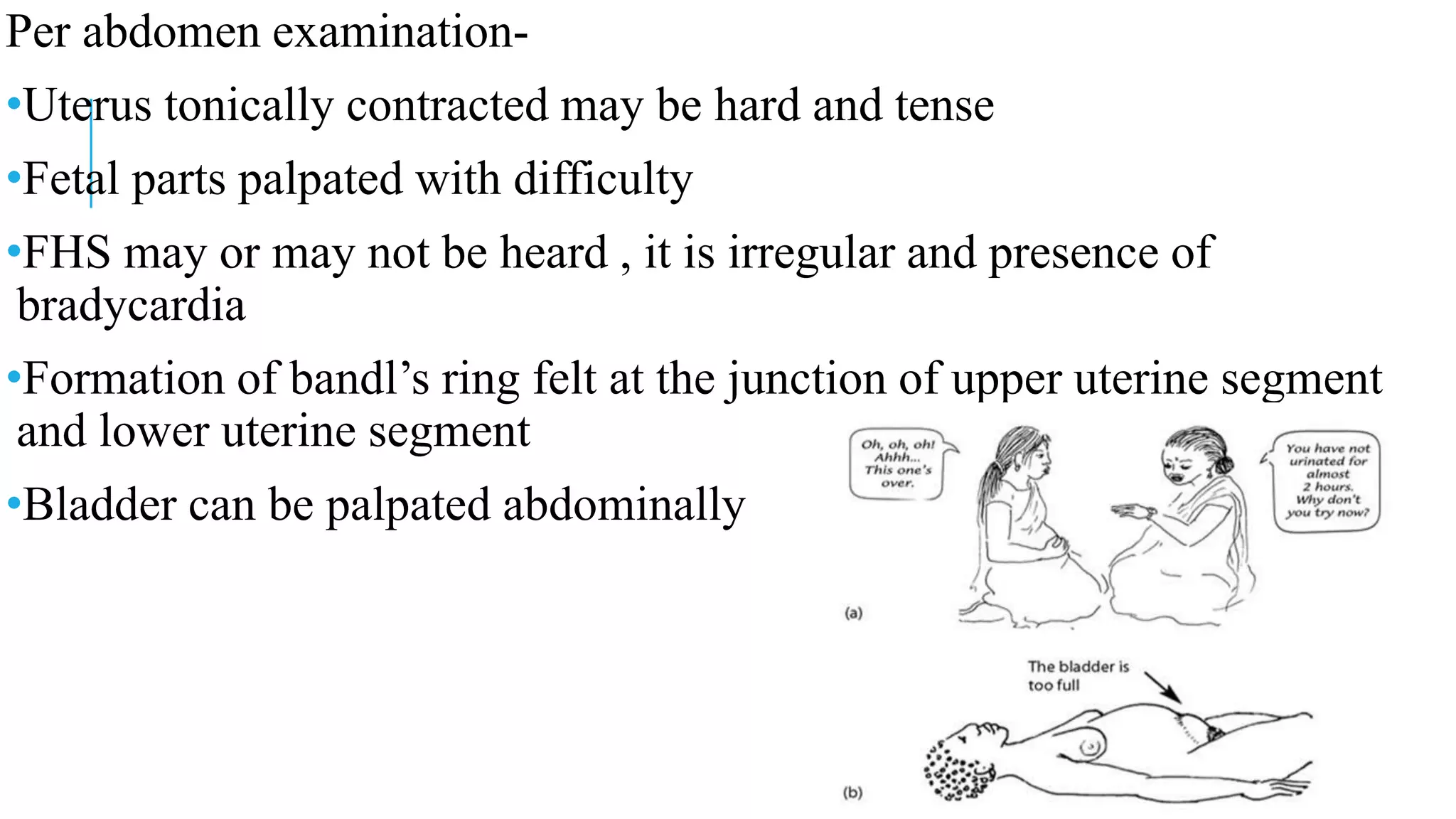
Obstructed labor is defined as the failure of the presenting part to descend despite good contractions due to mechanical obstruction, affecting 1-2% of cases in referral hospitals and contributing to 8% of maternal deaths globally. Causes include passenger-related issues like macrosomia and malpresentations, as well as passage-related obstructions such as cephalopelvic disproportion. Immediate management focuses on relieving the obstruction, ensuring maternal and fetal well-being, and preventing complications, with options including caesarean delivery or vaginal extraction under specific conditions.