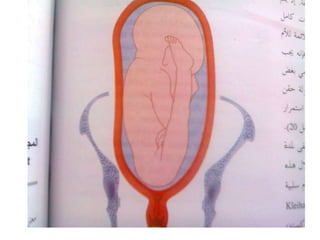
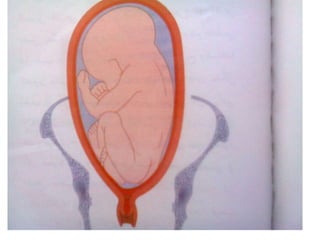
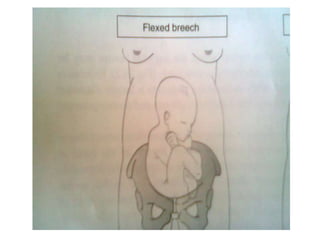
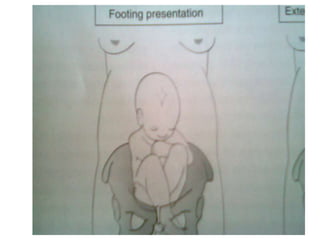
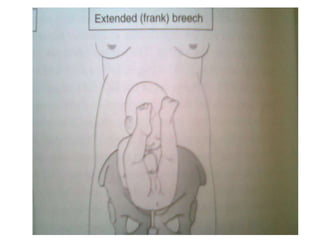
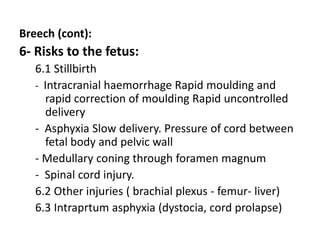
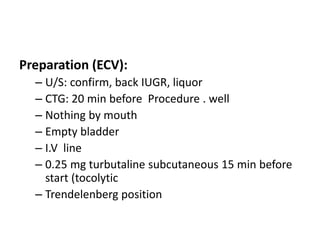
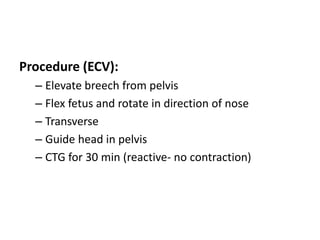
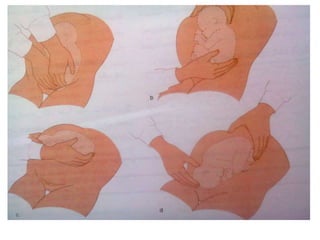
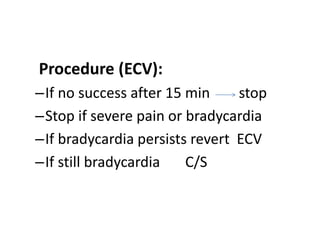
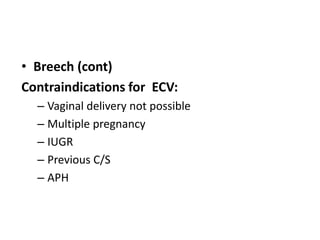
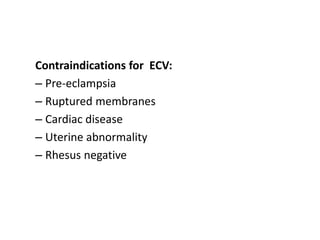
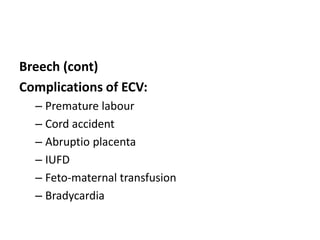
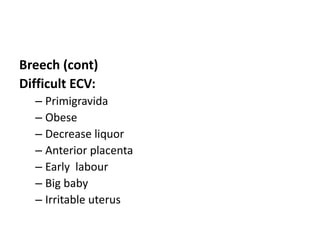
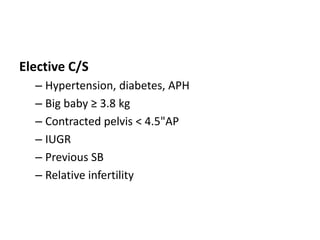
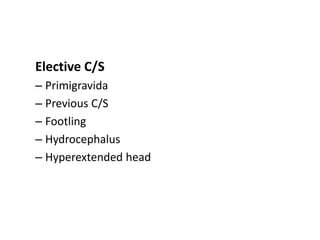
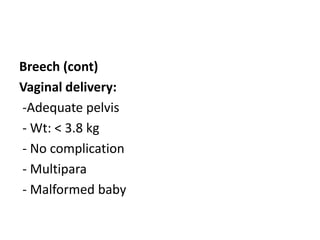
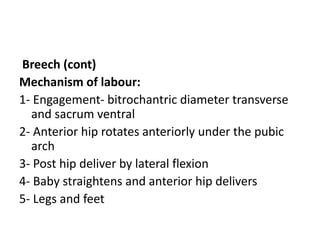
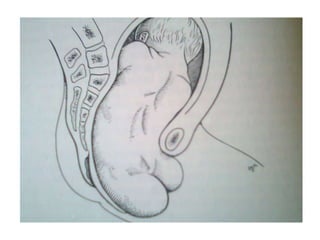
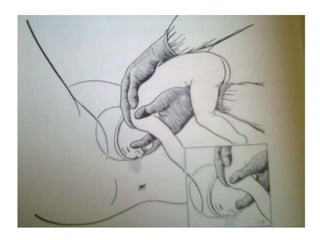
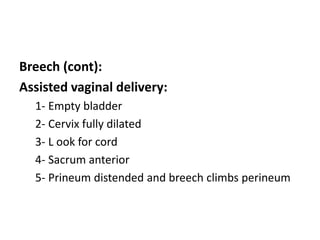
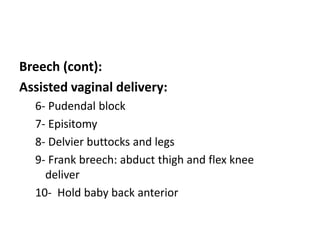
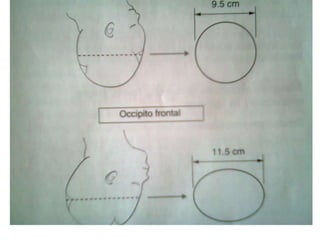
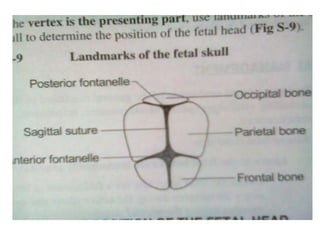
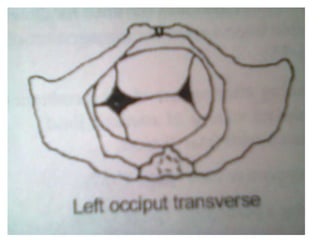
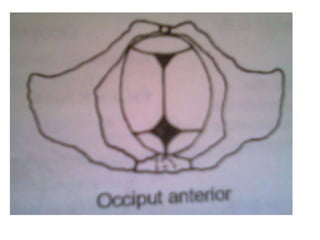
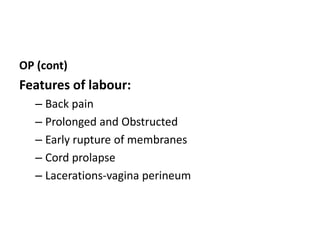
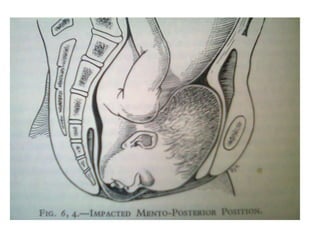
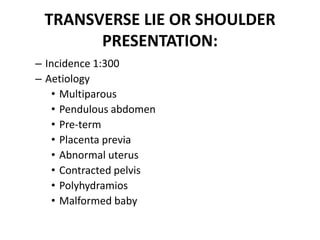
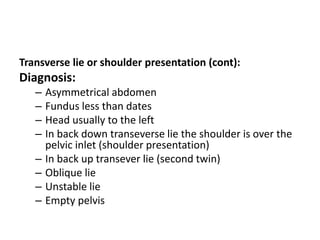
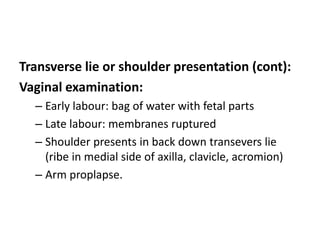
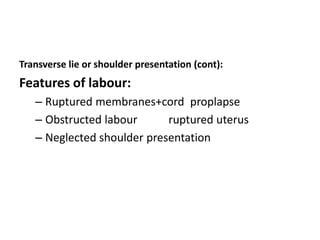
The document provides a comprehensive overview of malpresentation and malposition in childbirth, detailing definitions, risks to mother and fetus, predisposing factors, and specific conditions like breech, occipito posterior, and face presentations. It outlines management strategies including early diagnosis, monitoring, and various delivery methods depending on the presentation type and associated risks. Emphasis is placed on the importance of trained attendants and appropriate facilities to mitigate complications during labor.