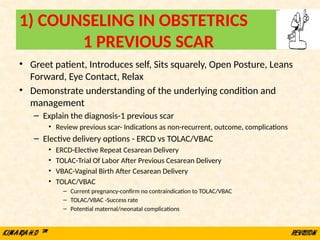
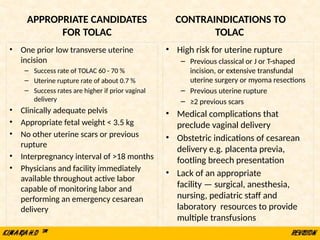
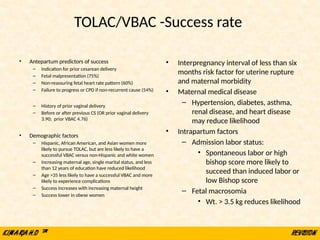
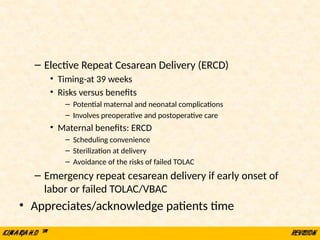
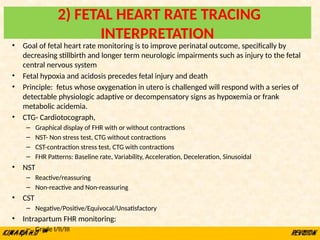
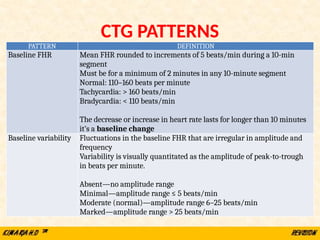
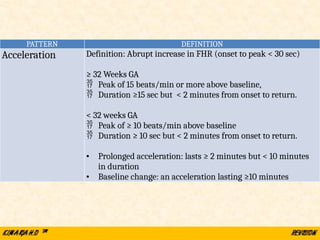
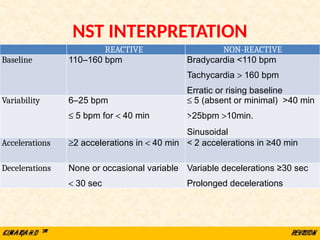
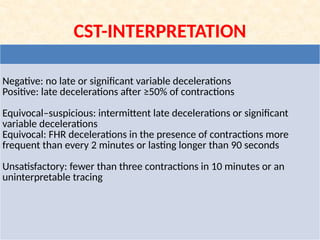
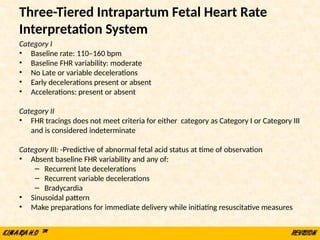
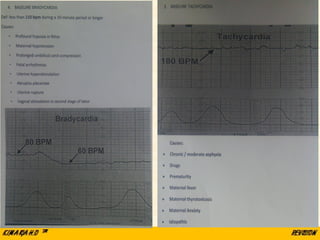
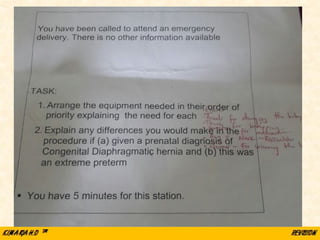
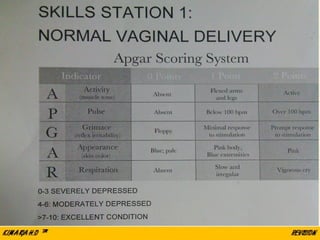
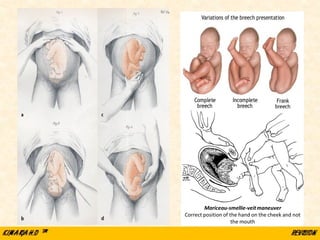
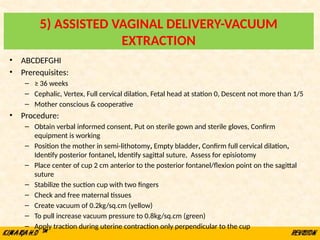
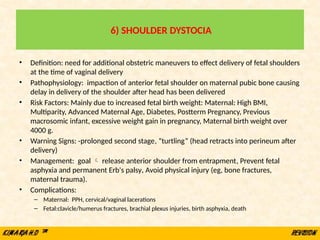
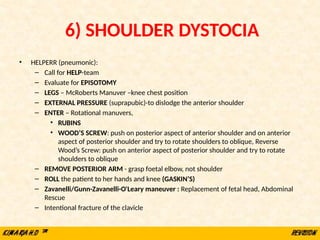
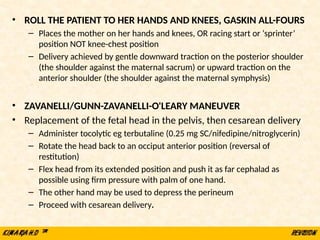
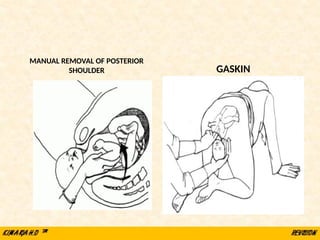
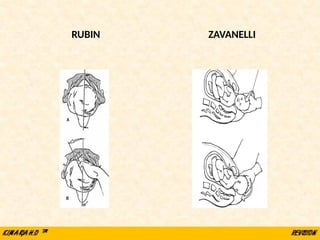
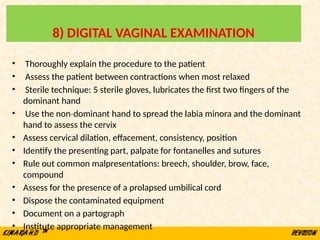
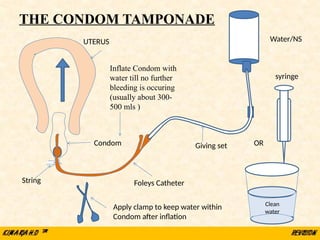
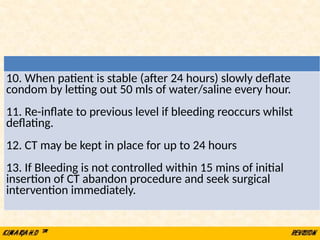
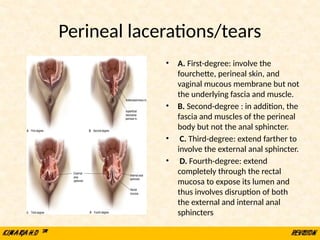
The document outlines essential obstetric skills for medical practitioners, covering various procedures and techniques including counseling for previous cesarean scars, fetal heart rate monitoring, vaginal deliveries (normal and breech), assisted vaginal deliveries, and management of complications like shoulder dystocia. It emphasizes the importance of understanding patient history and effective communication in managing risks associated with vaginal births after cesareans and other scenarios. Detailed procedures, indications, contraindications, and potential complications for each skill are provided to ensure safe and effective practice.