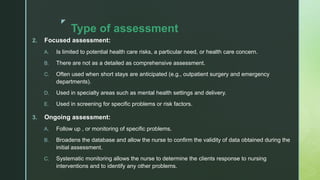
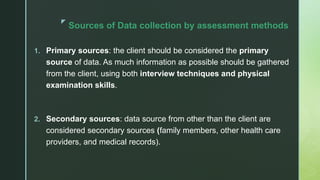
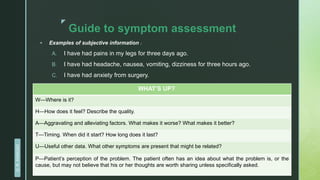
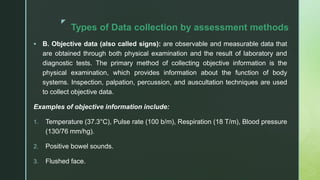
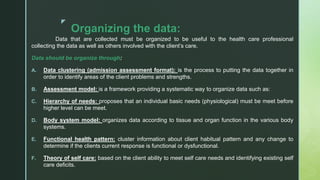
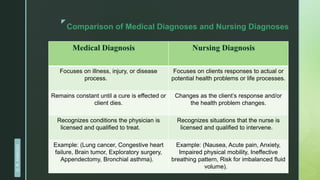
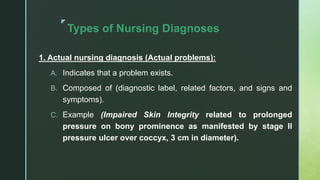
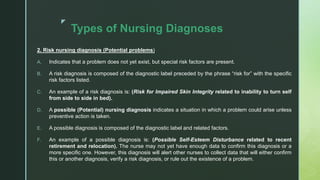
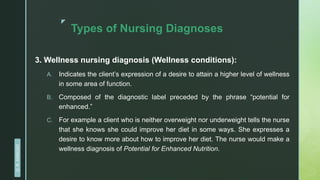
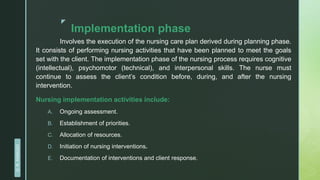
The document discusses the nursing process, which is a systematic method for planning and providing nursing care. It outlines the key steps as assessment, diagnosis, planning, implementation, and evaluation. Assessment involves collecting both subjective and objective data from various sources like the client, family, and medical records. This data is then organized, interpreted, and documented. The nursing diagnosis phase further analyzes the collected data to identify any actual or potential health problems nurses can address. The overall nursing process provides structure to nursing care and allows for continuity and quality of care.