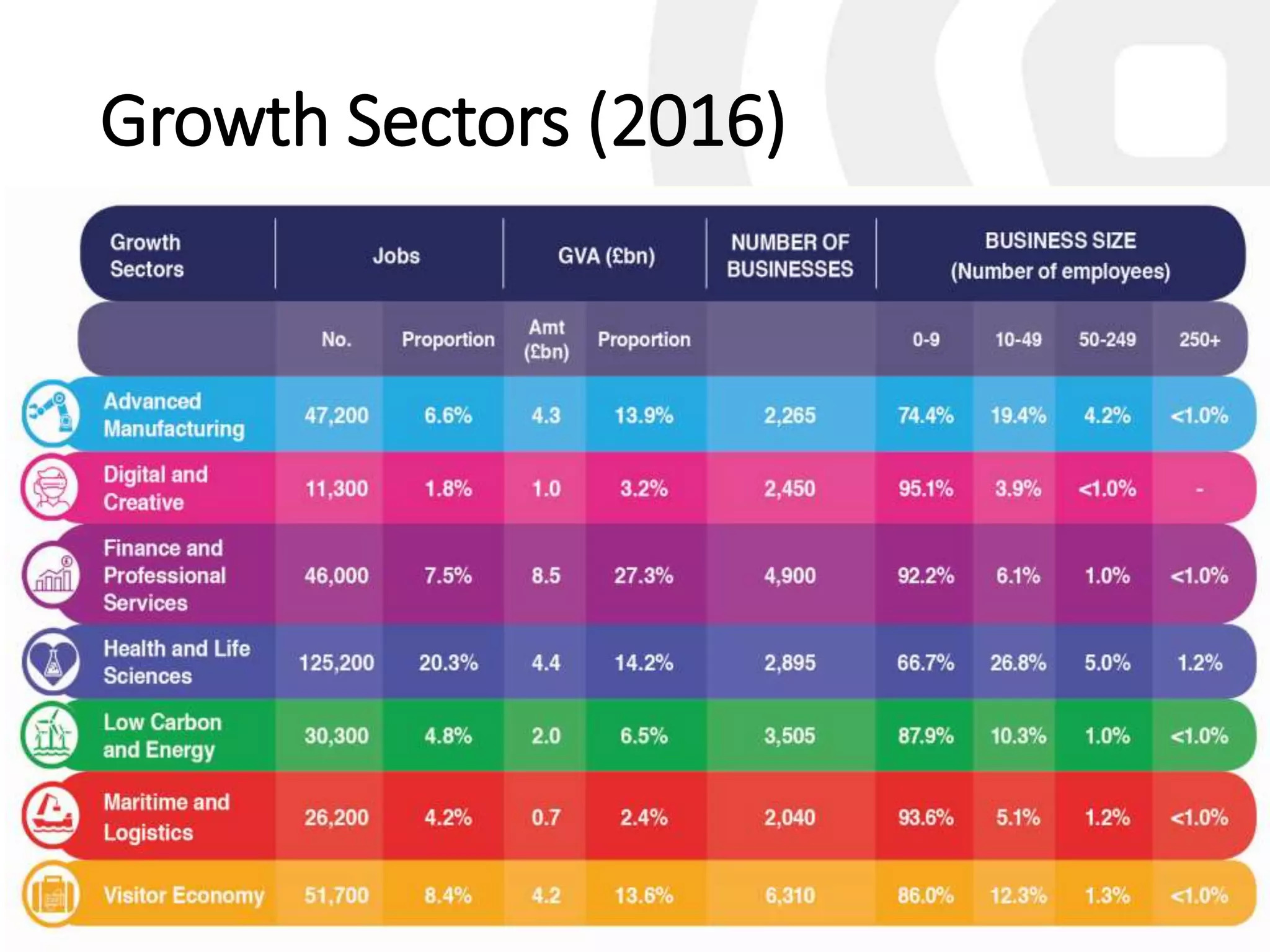
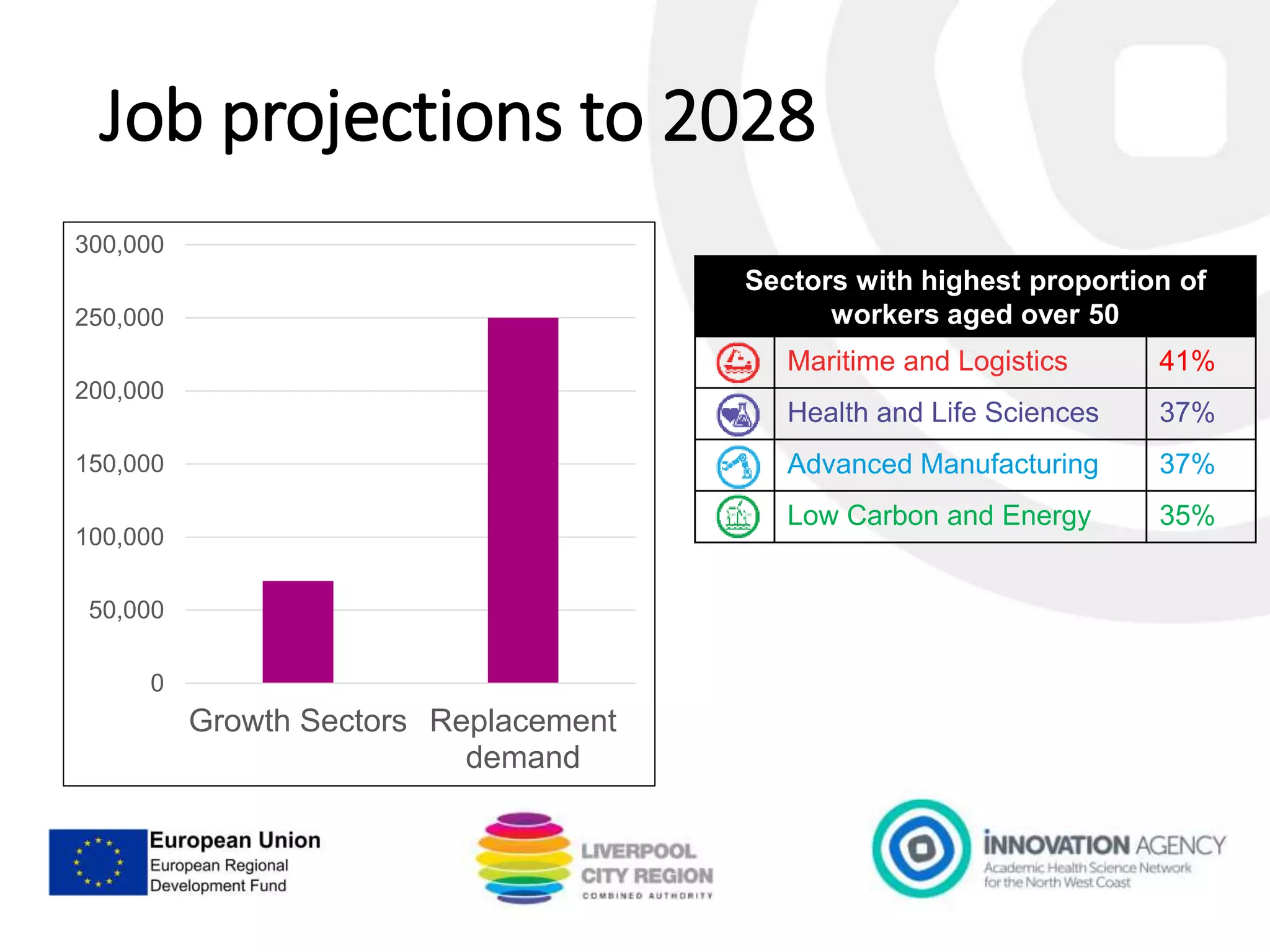
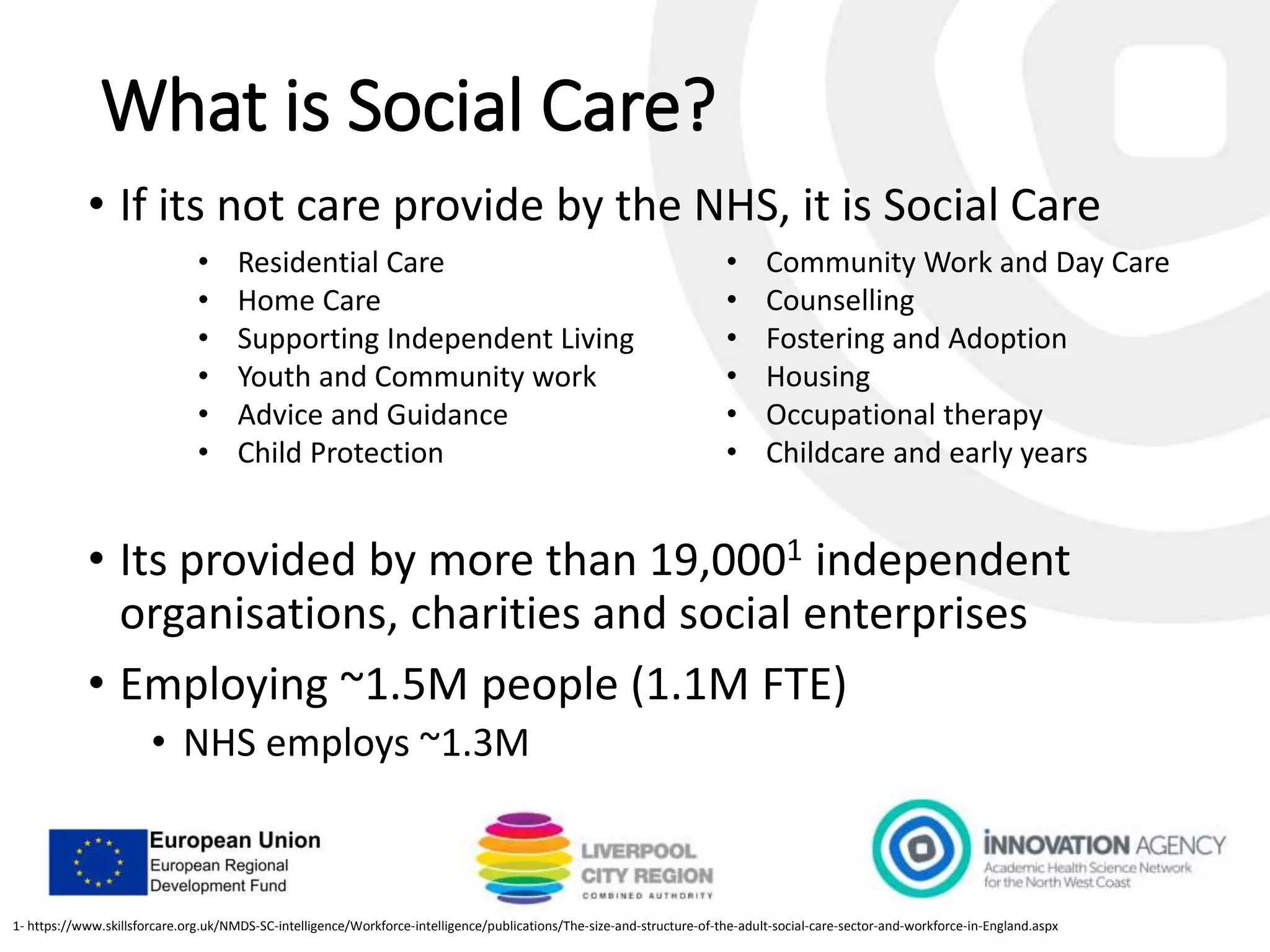
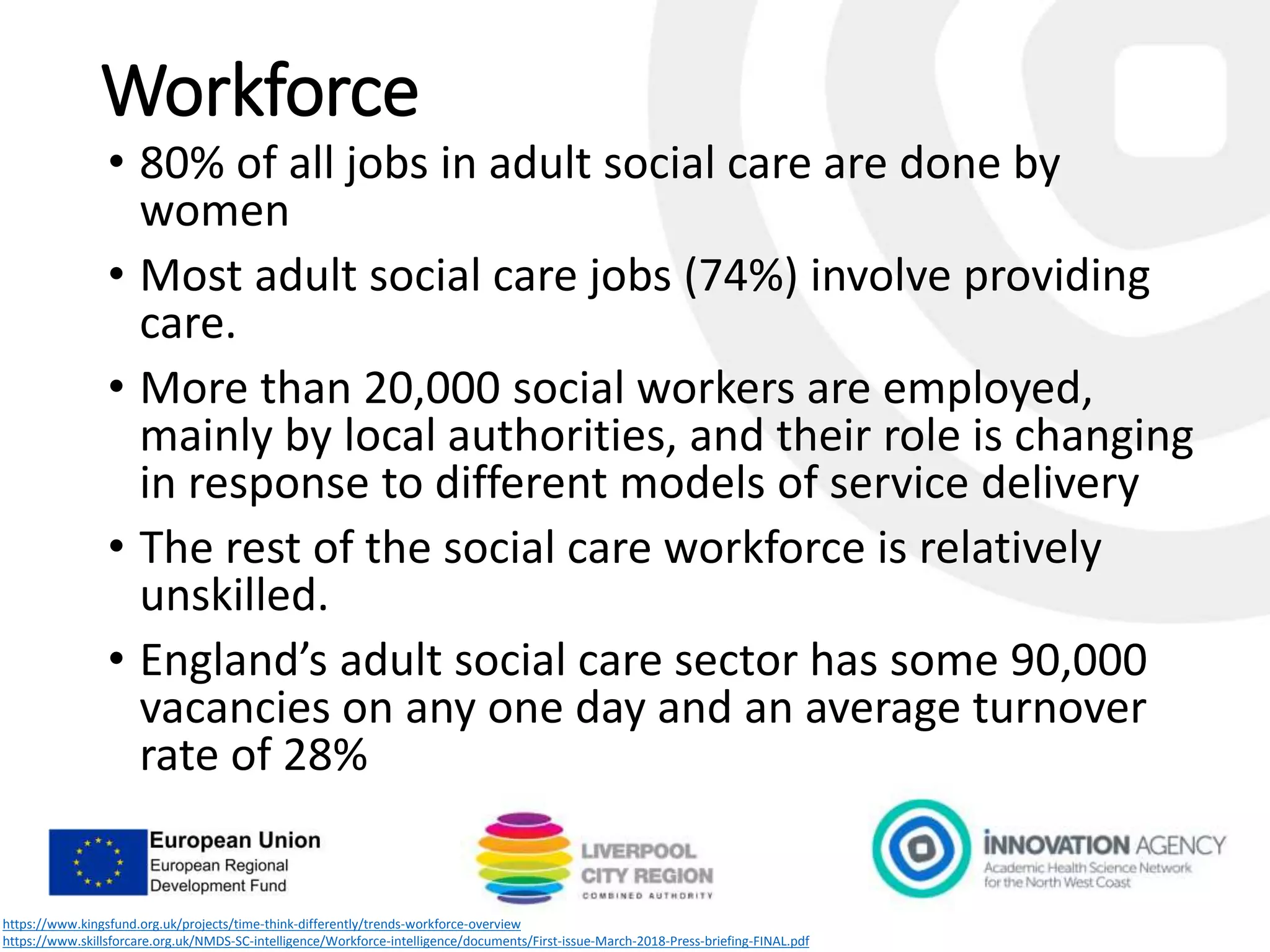
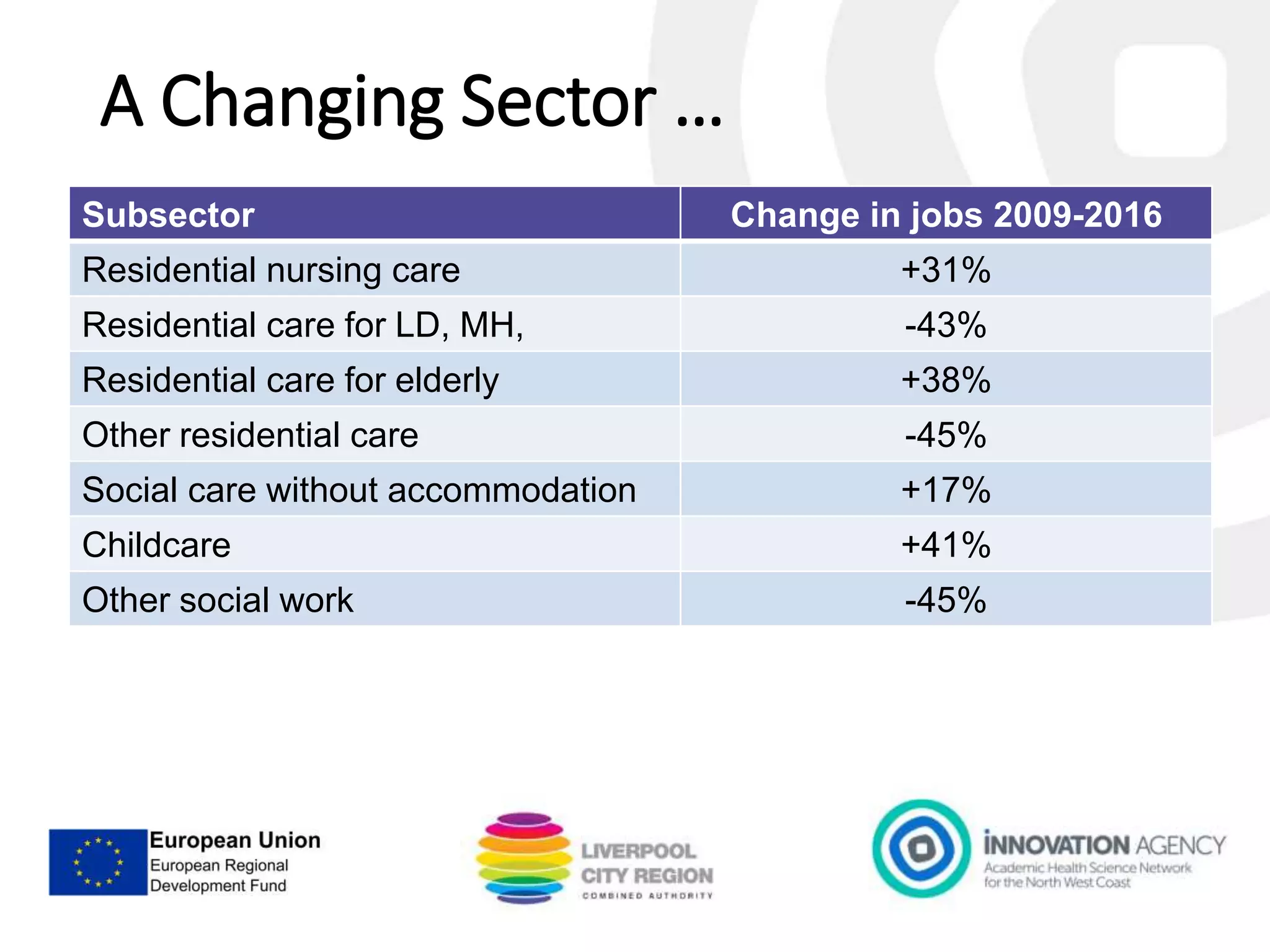
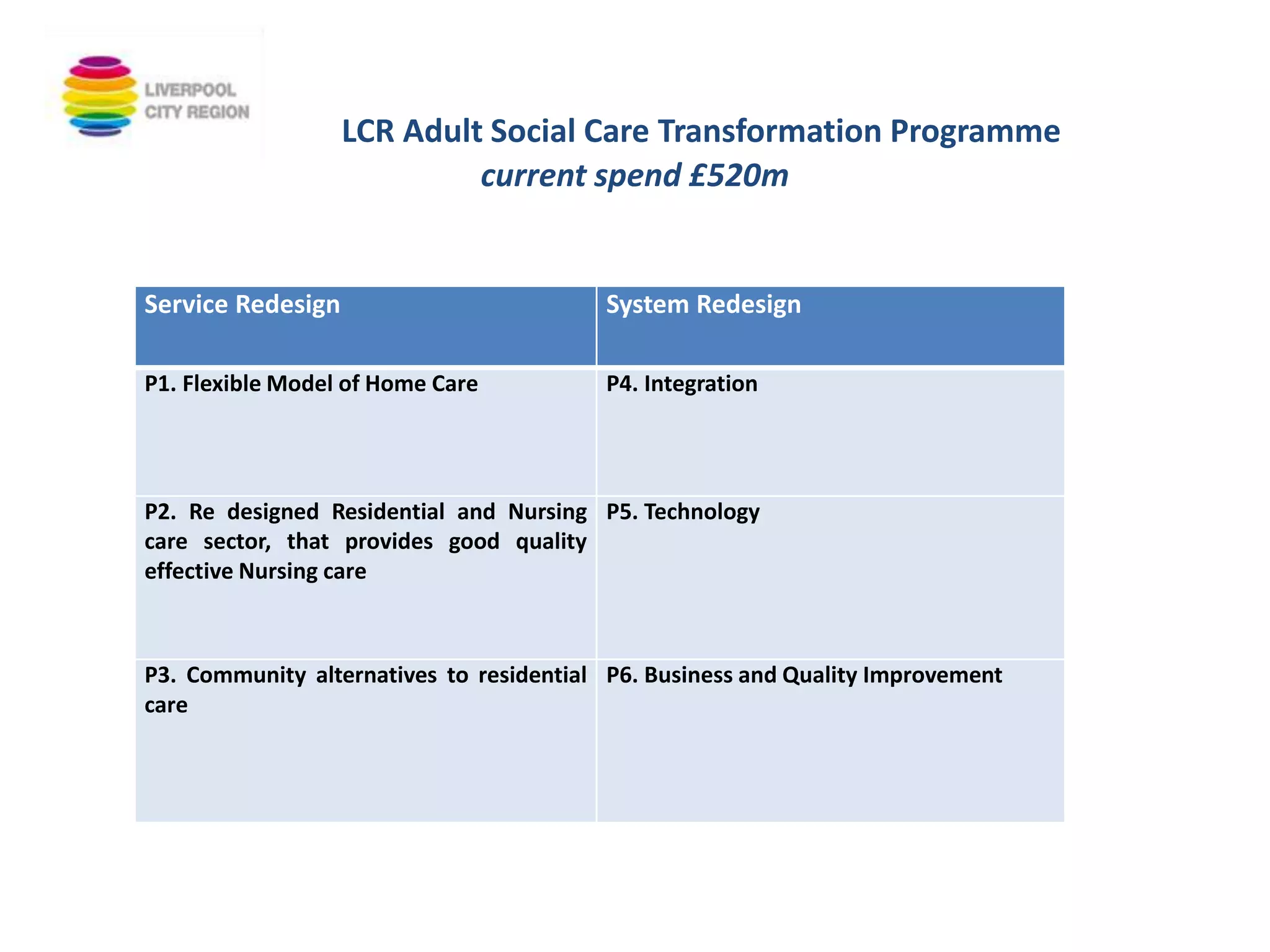
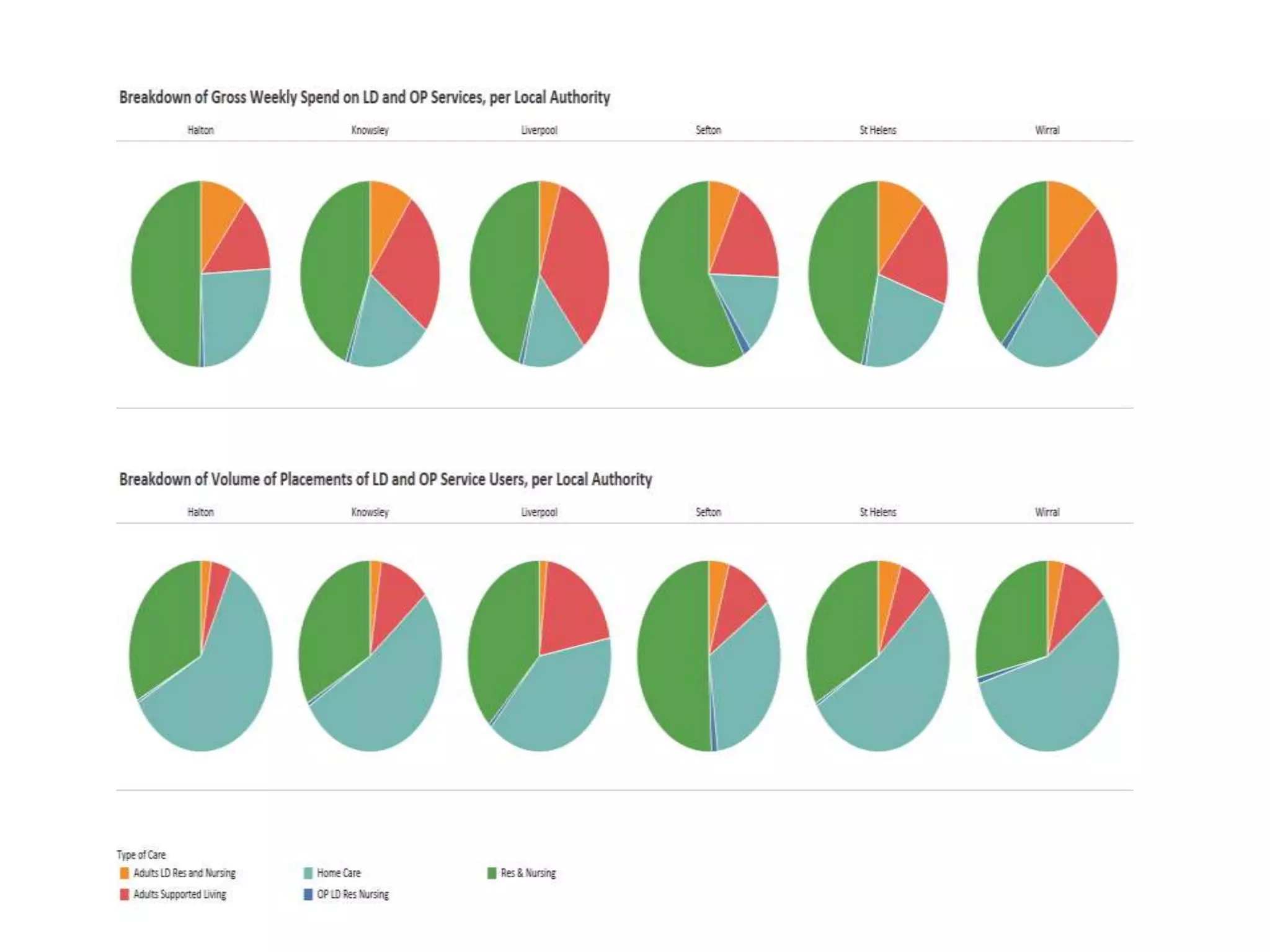
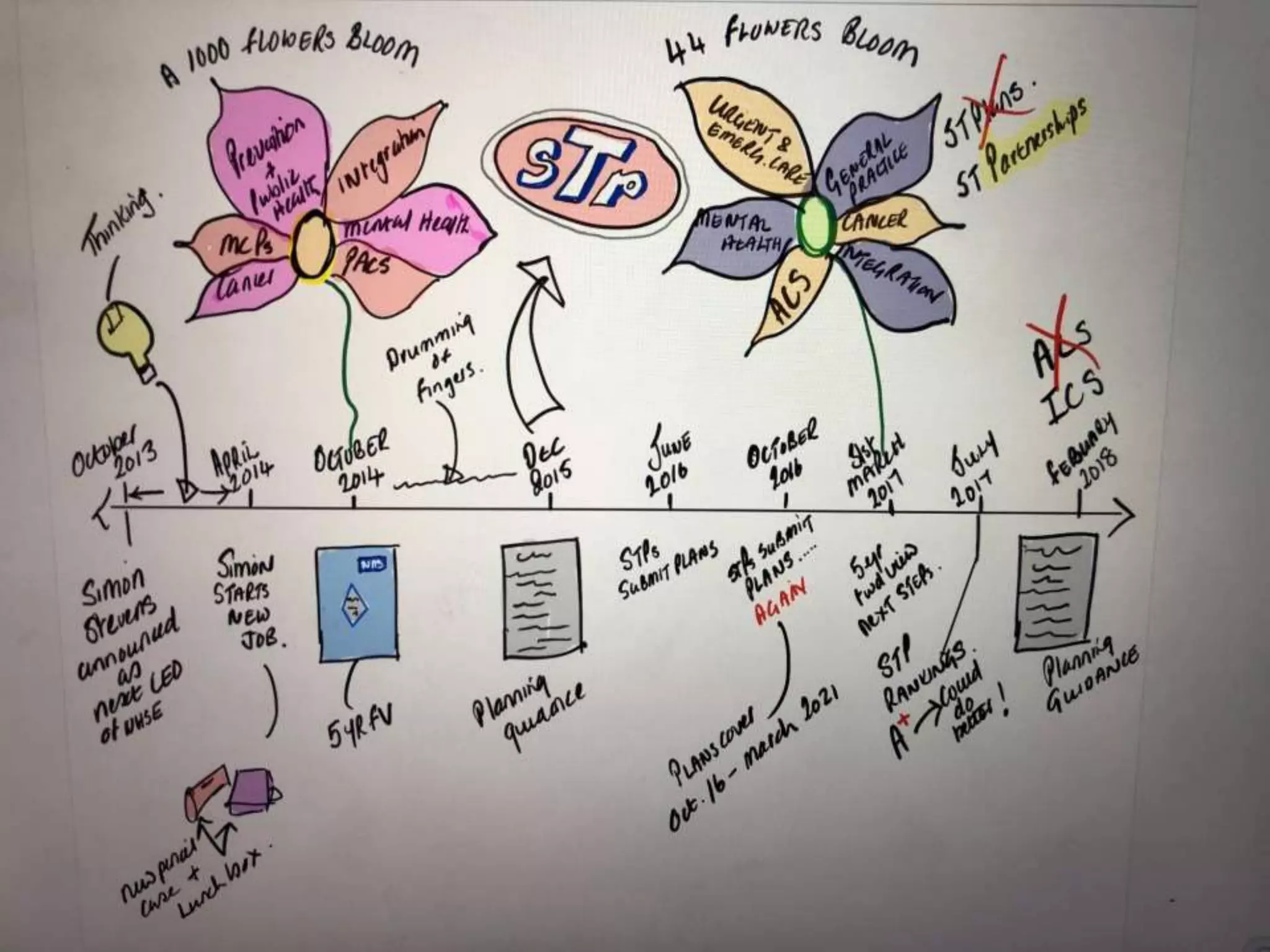
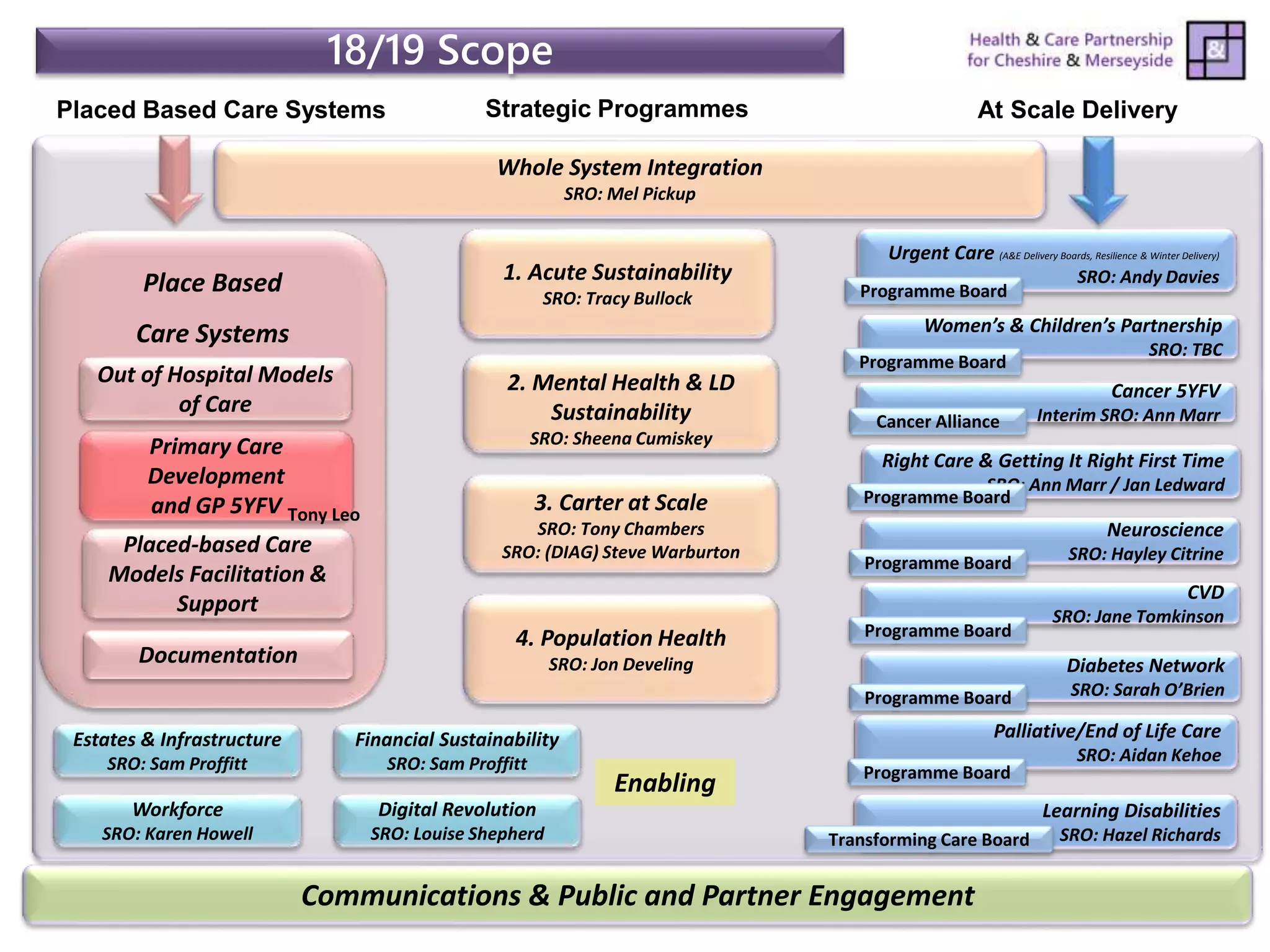
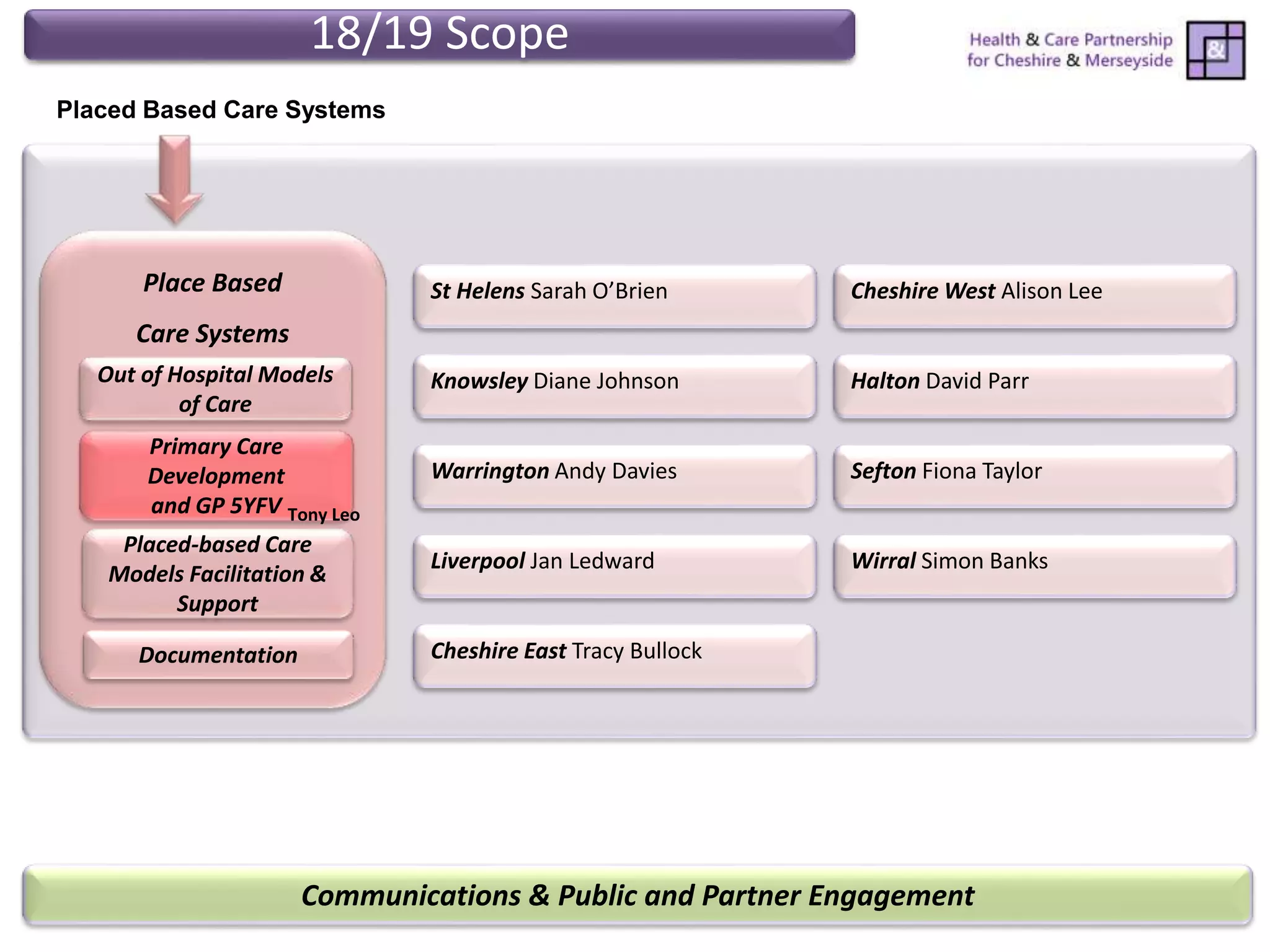
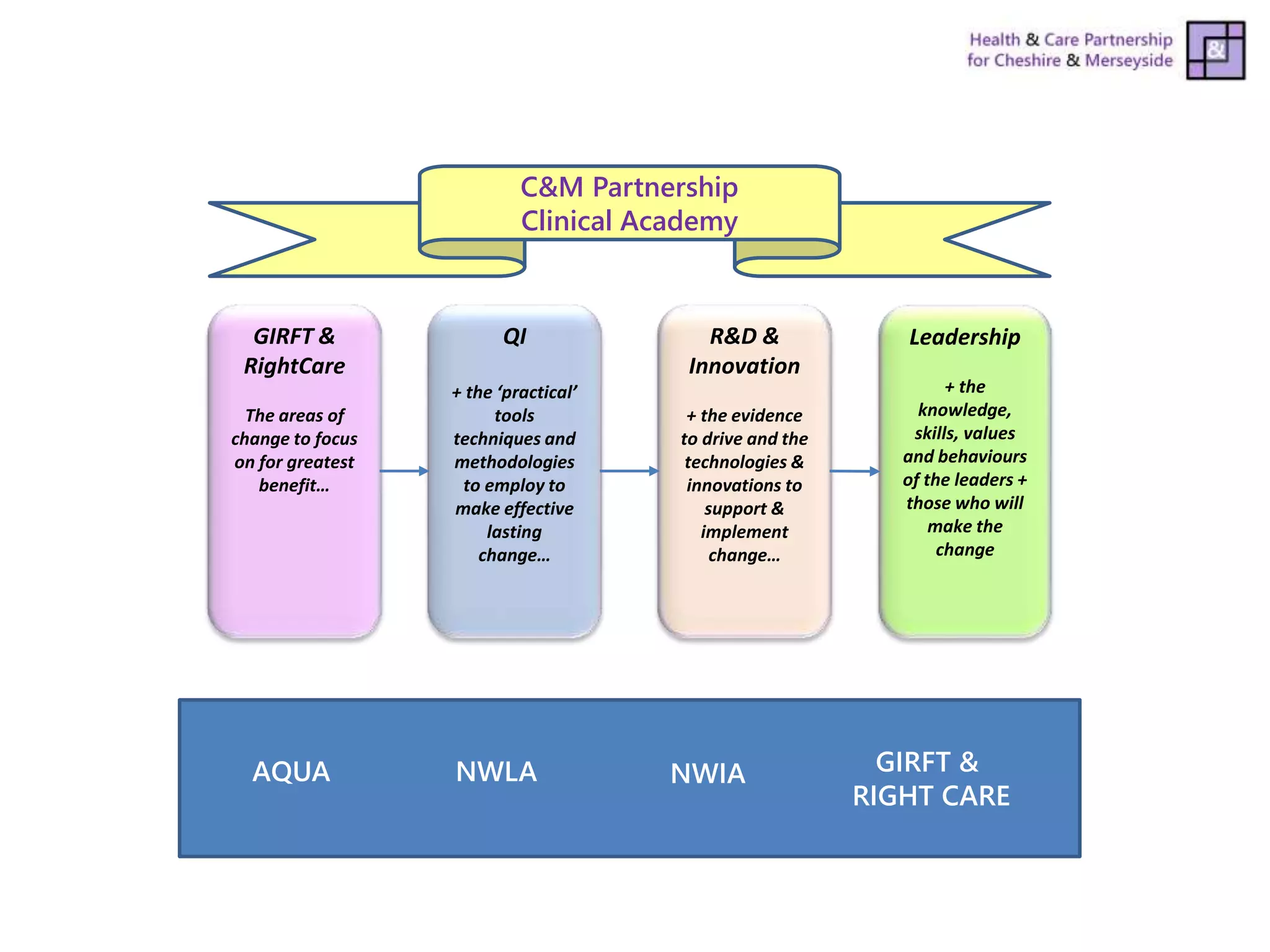
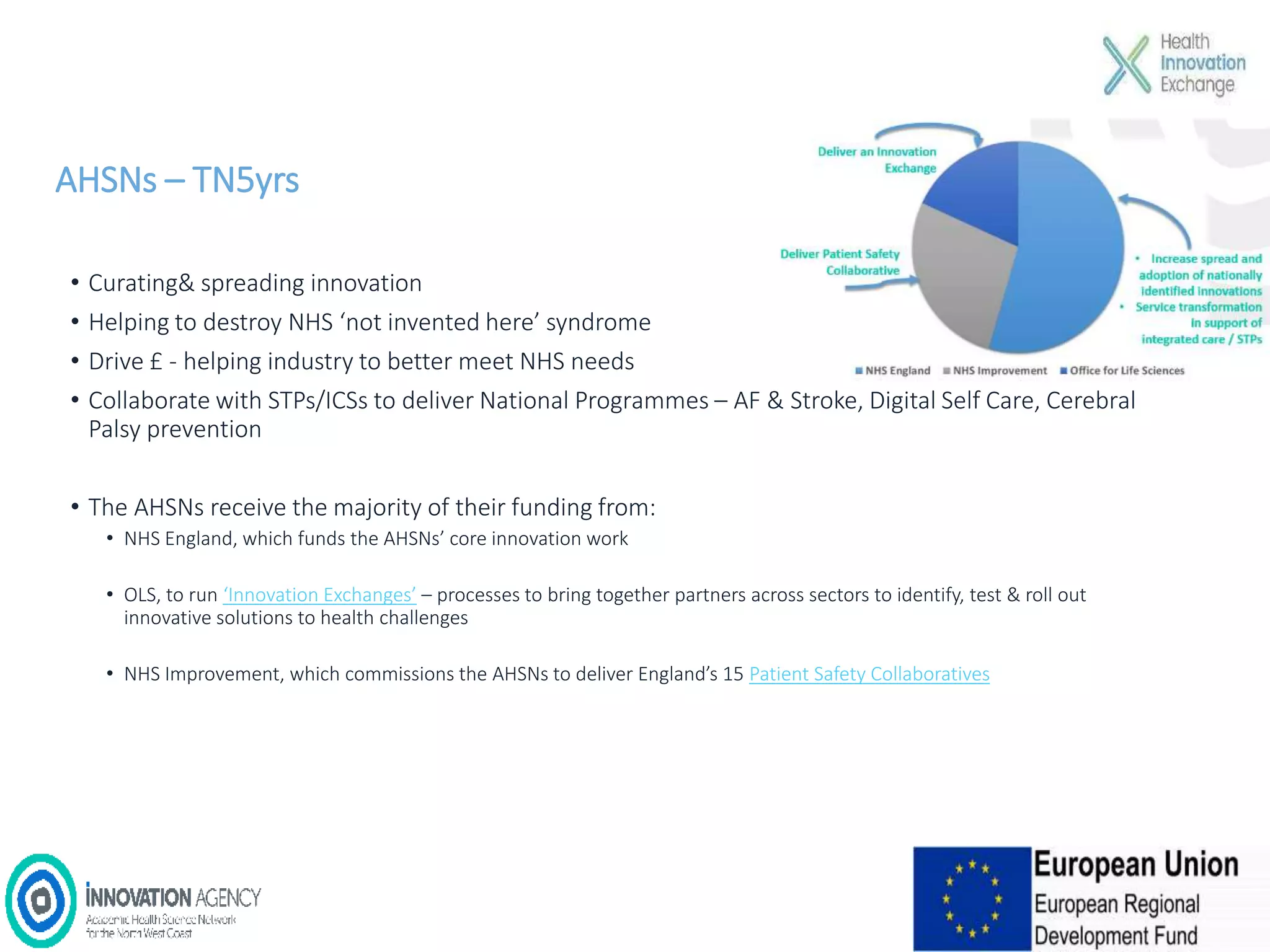
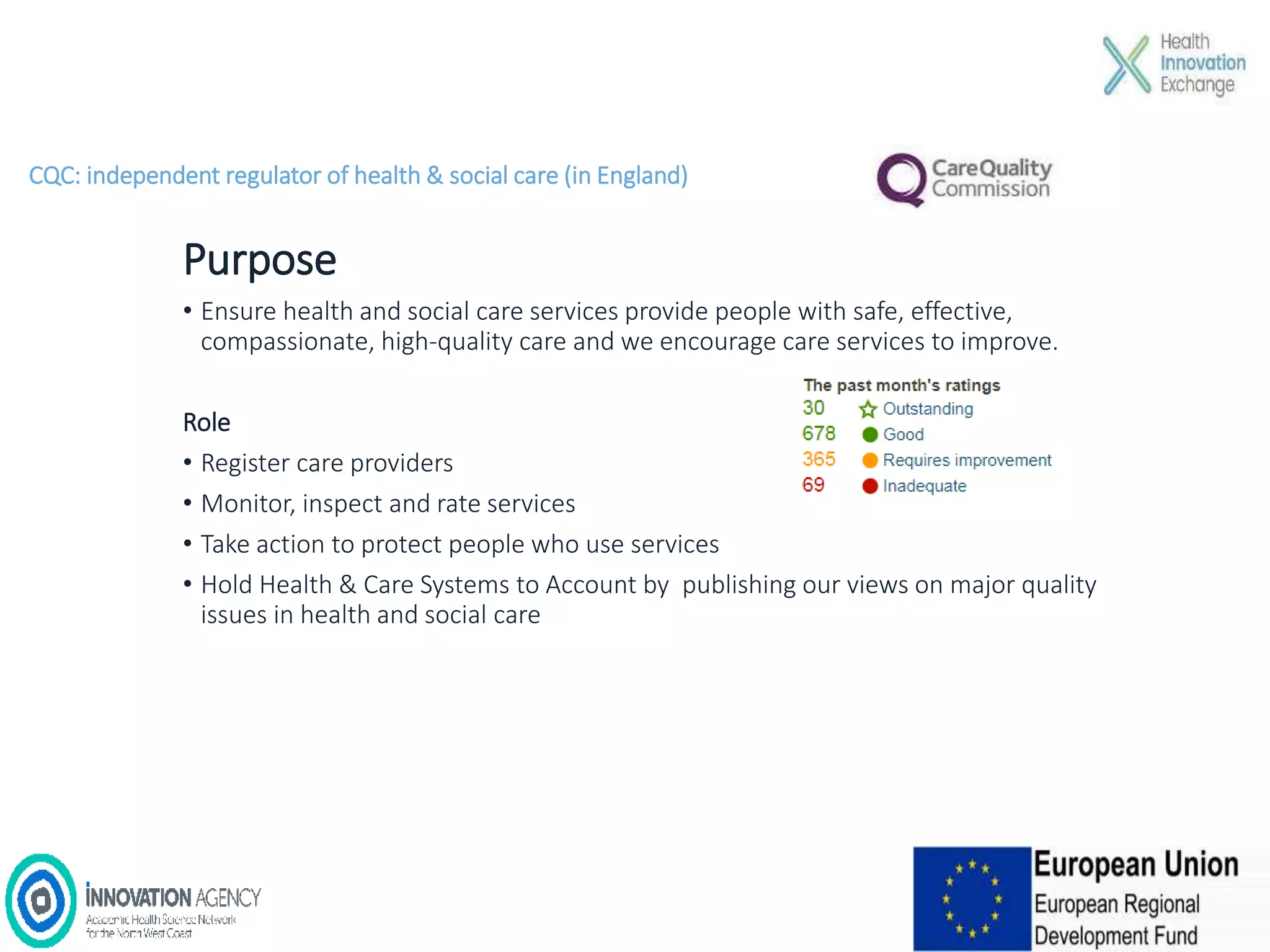
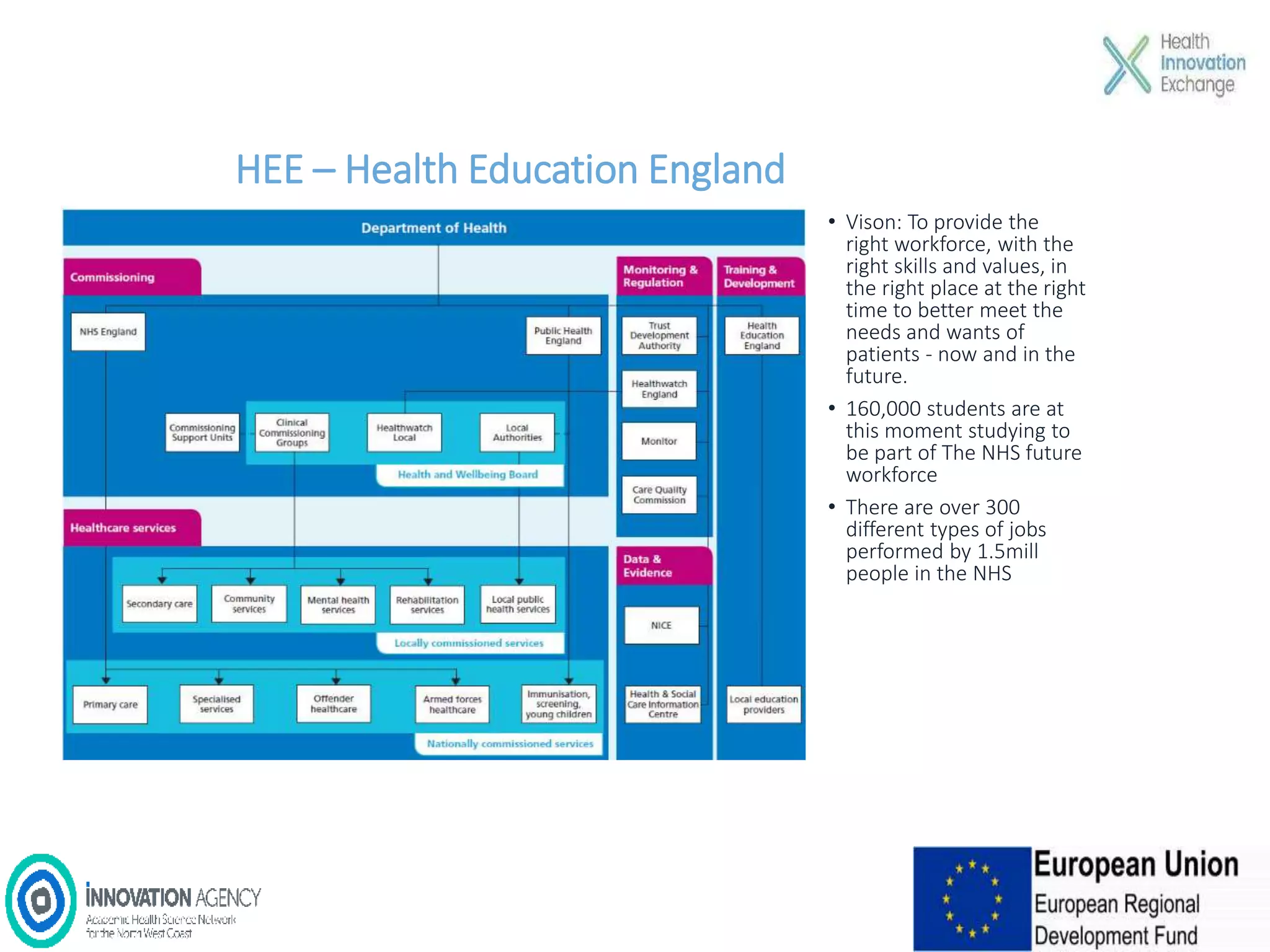
The workshop on September 11, 2018, discussed the NHS and social care structures, priorities, and commissioning in the Liverpool City Region. Key topics included the NHS overview, funding challenges, social care integration, workforce issues, and the role of various health organizations in improving care delivery. Emphasis was placed on collaboration, prevention strategies, and utilizing technology to address health disparities and enhance service efficiency.