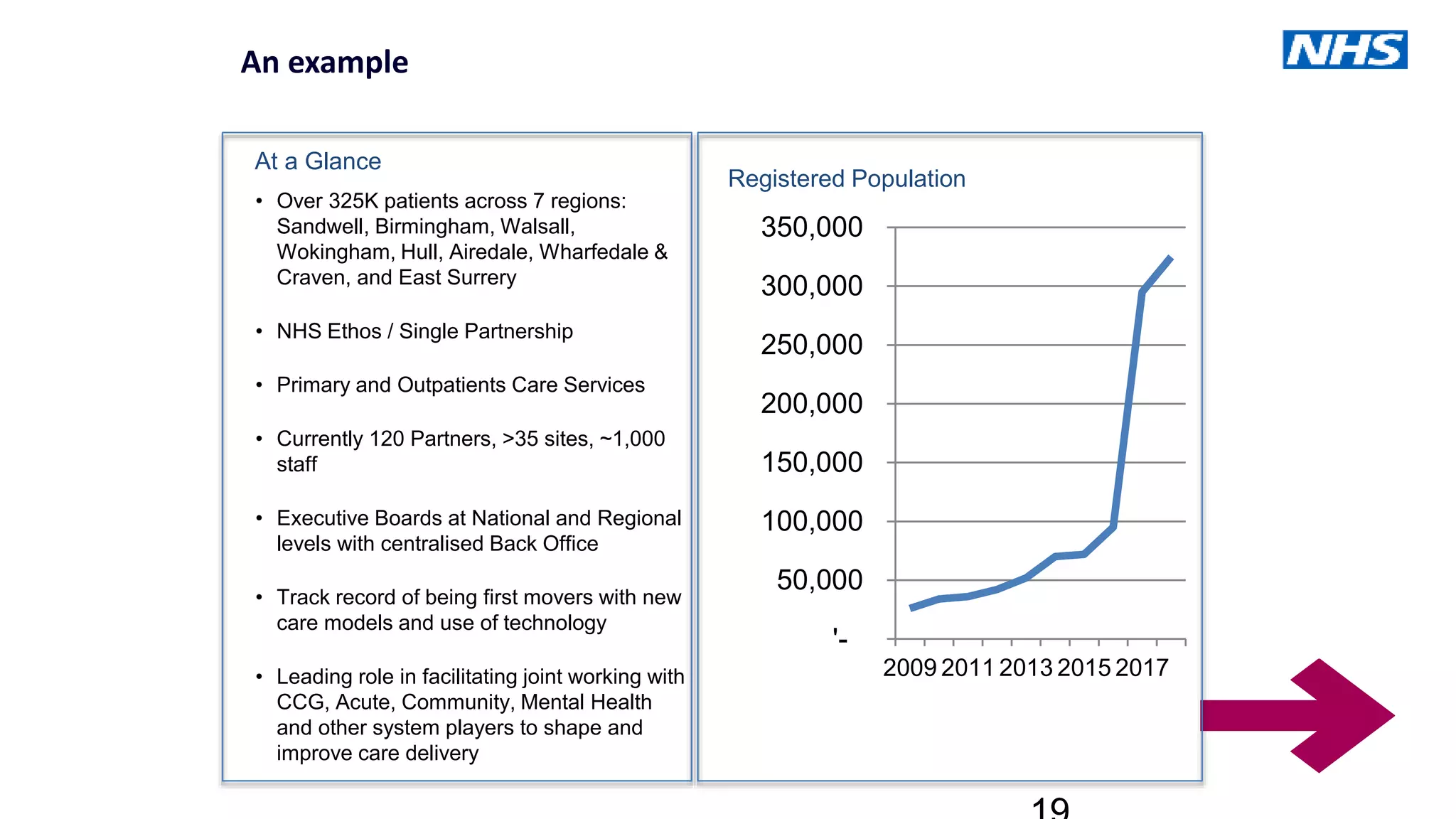
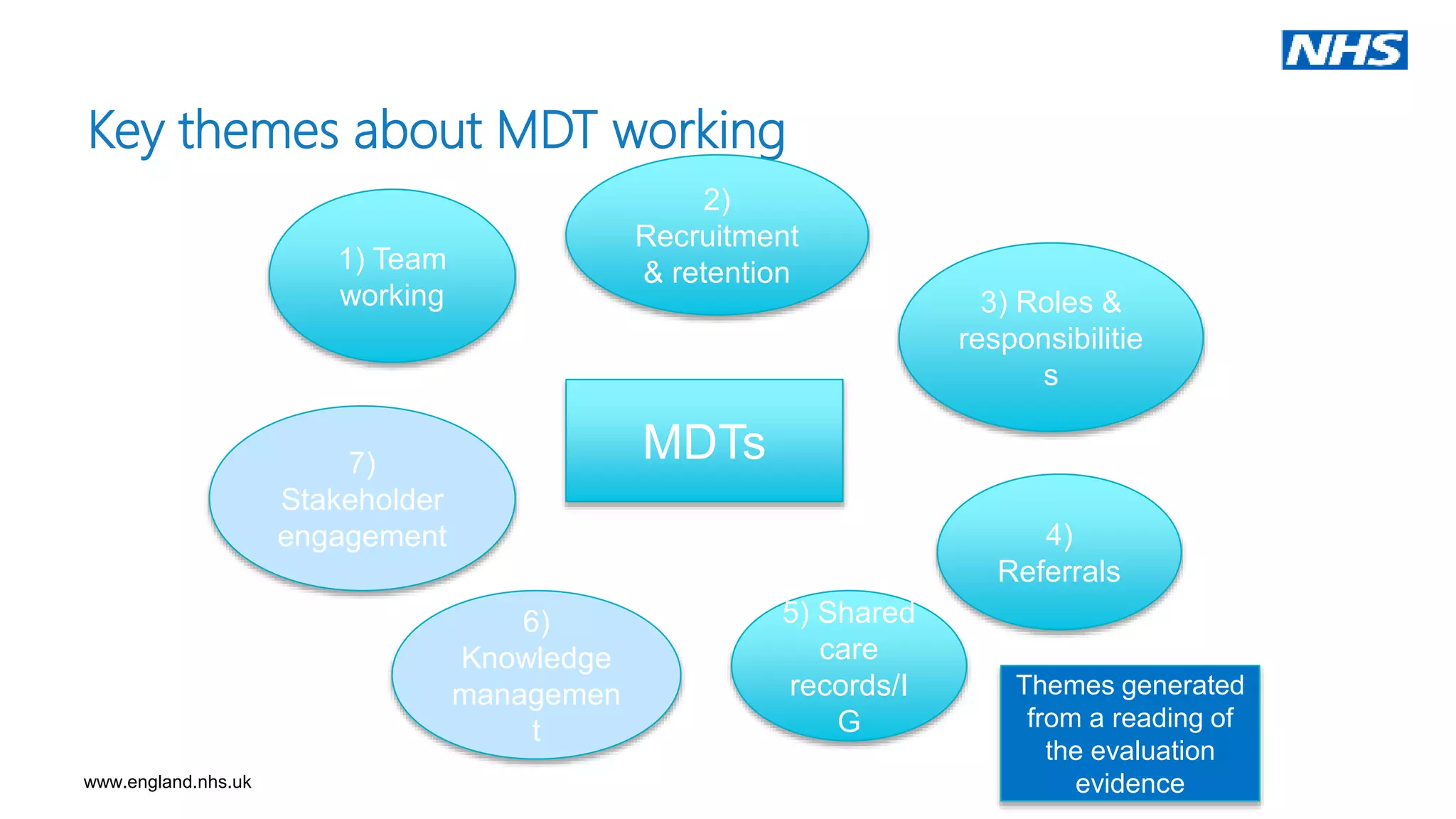
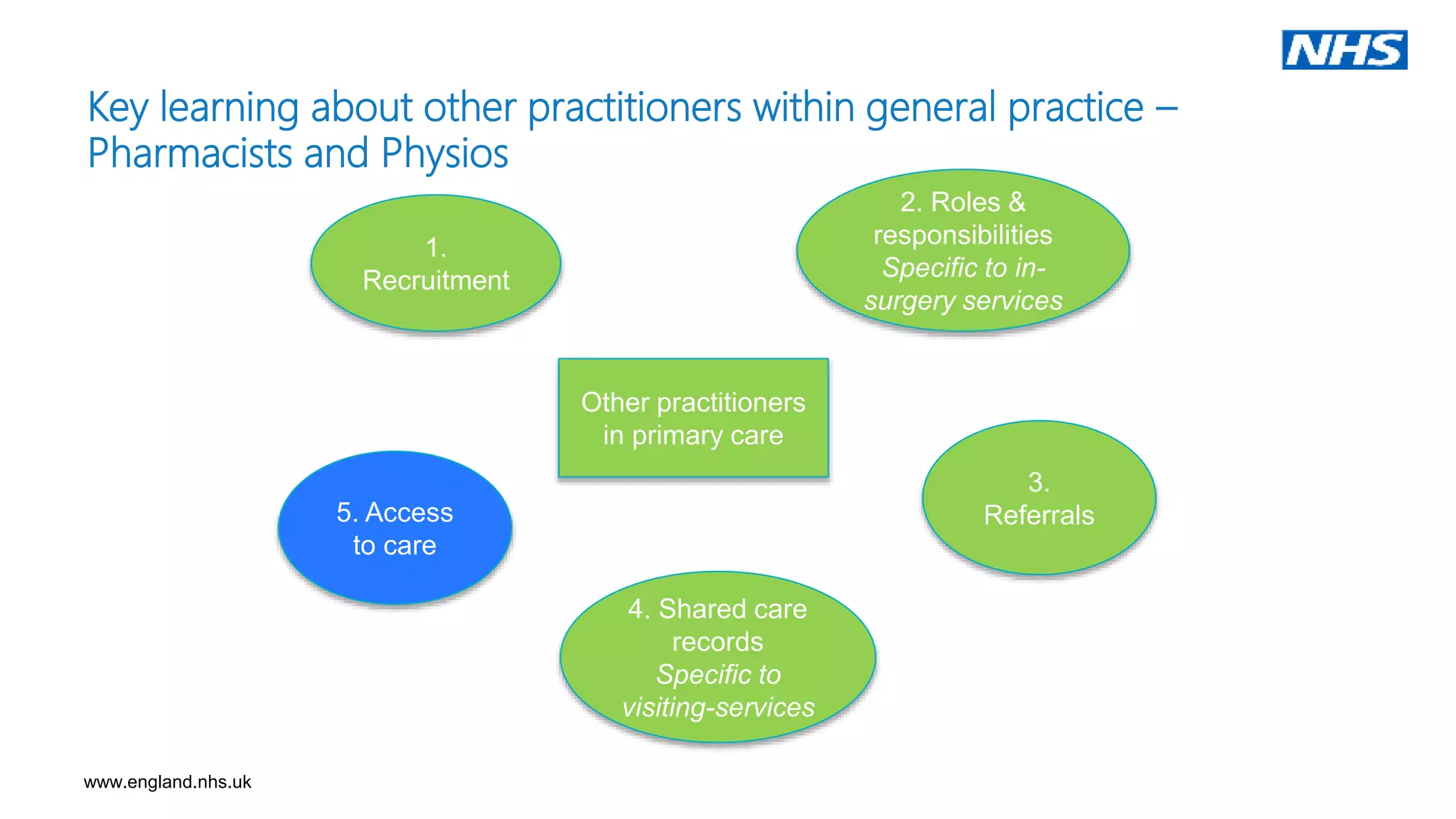
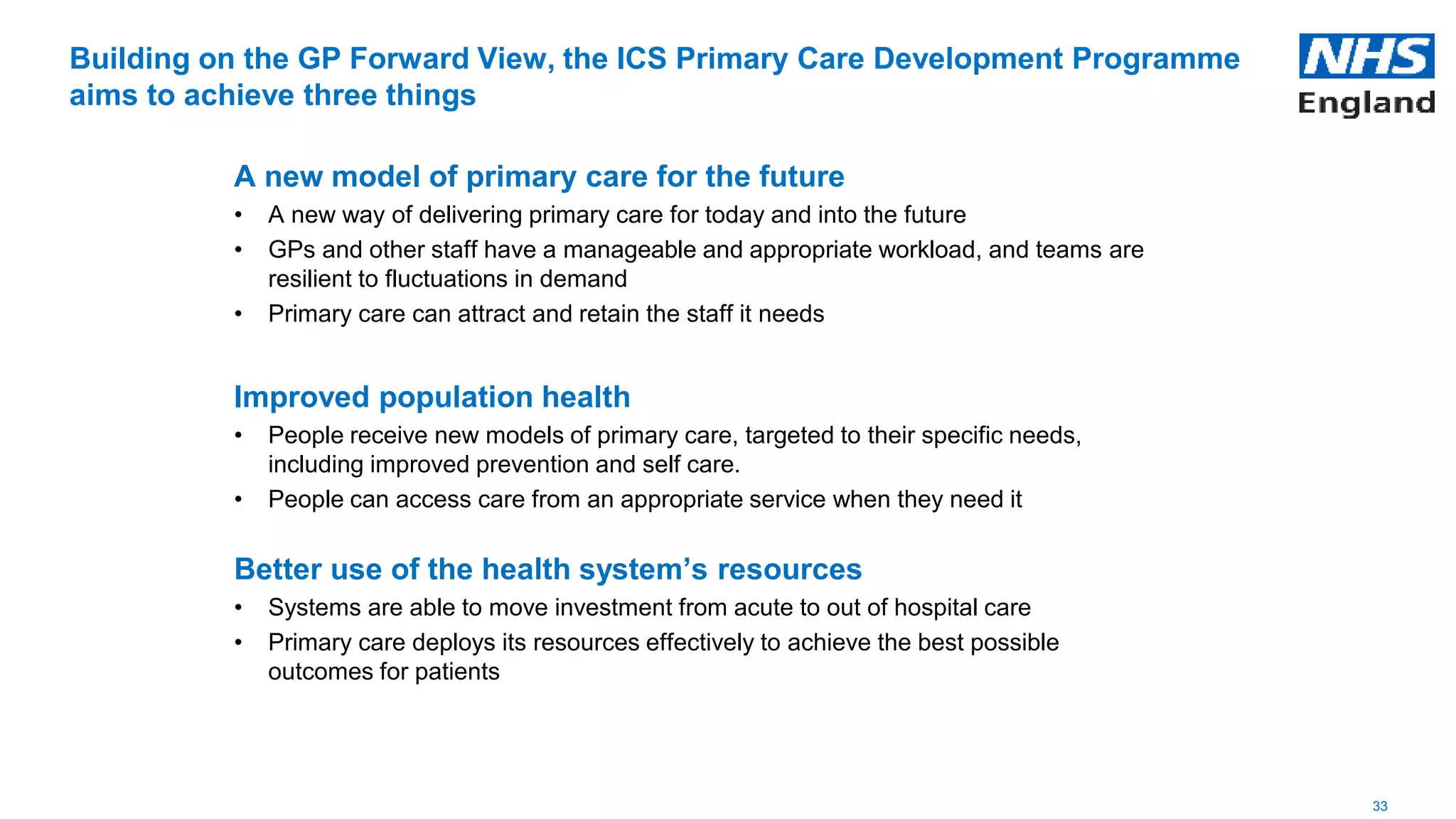
The document summarizes the key themes and learnings from the National ICS Primary Care Development Programme in the UK. The three main points are:
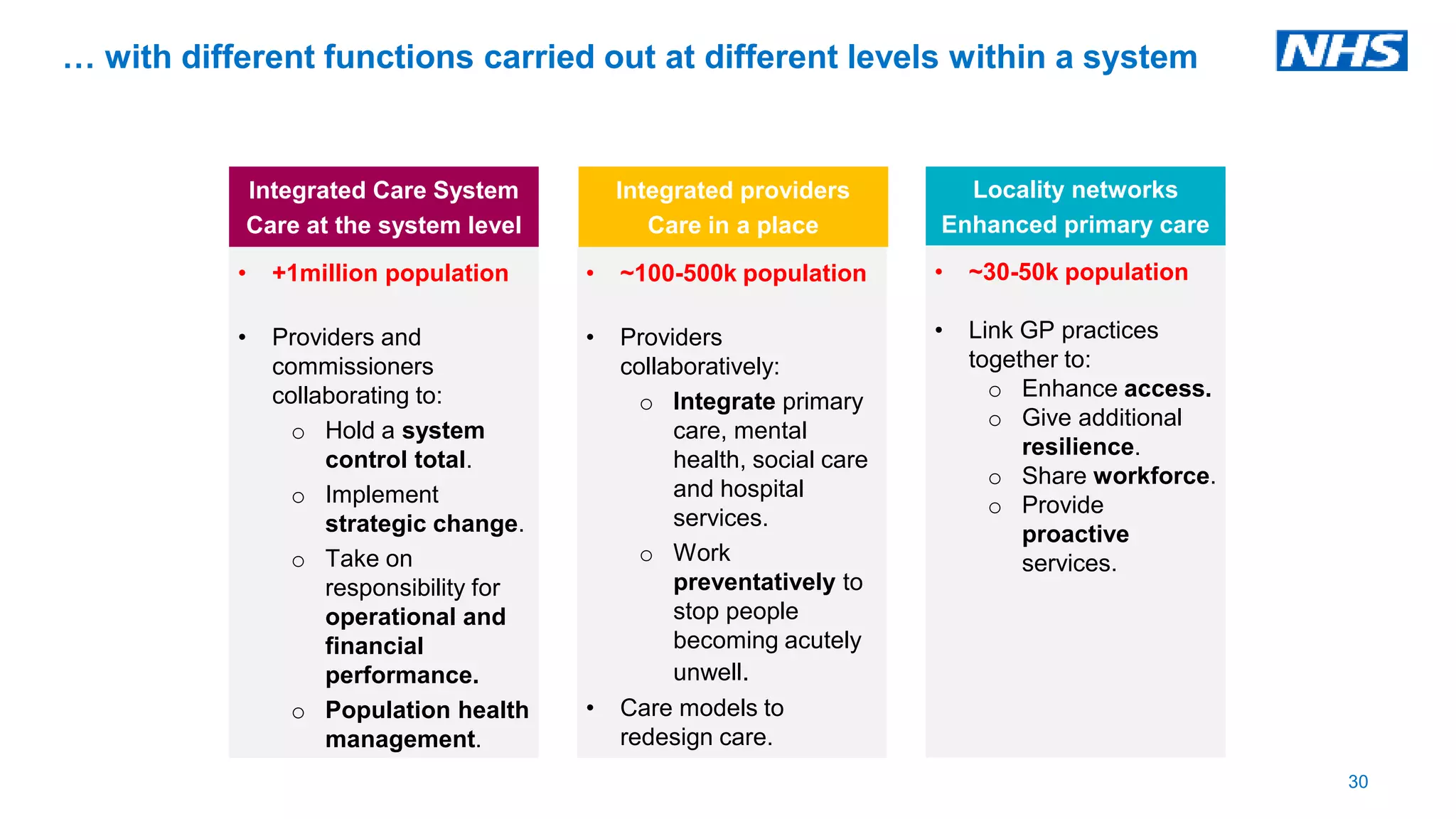
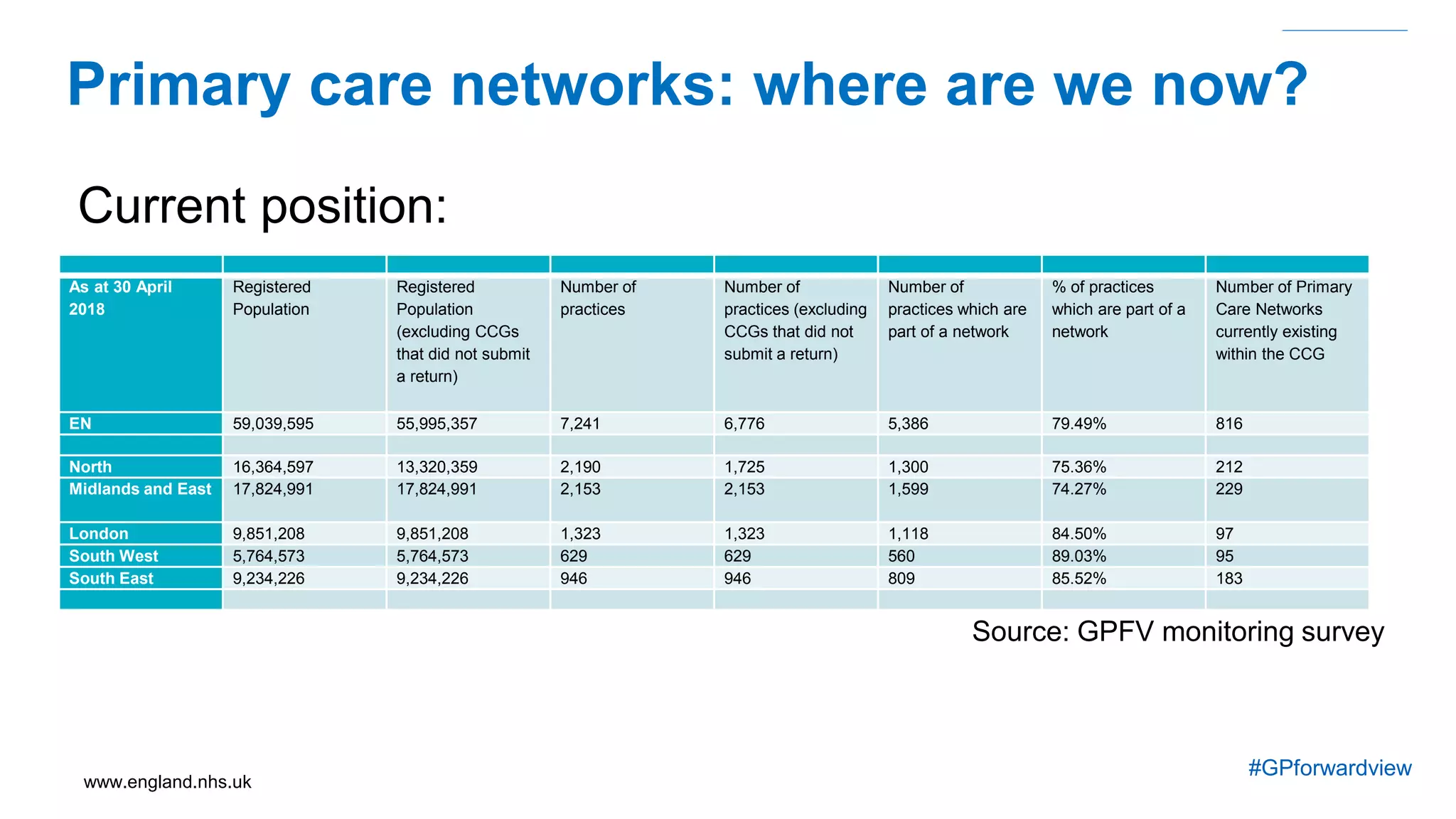
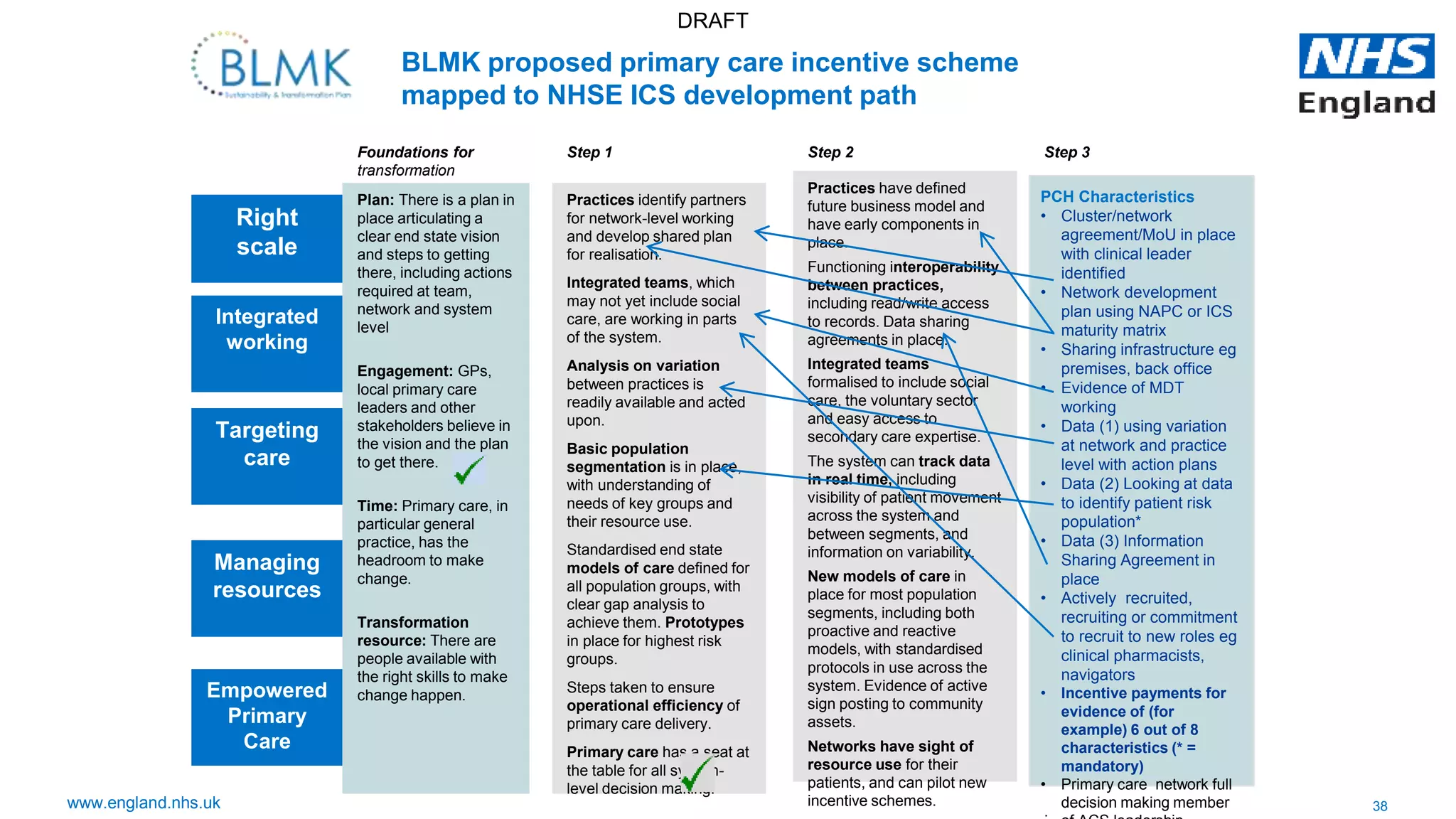
1) Primary care networks are being established to improve coordination of care across practices and community services for populations of 30,000-50,000 people. This allows for integrated working at the right scale.
2) Five themes are emerging around empowering primary care through equal partnerships, understanding population needs to target care, managing resources and reducing variation, integrated working across services, and networks working at the right scale.
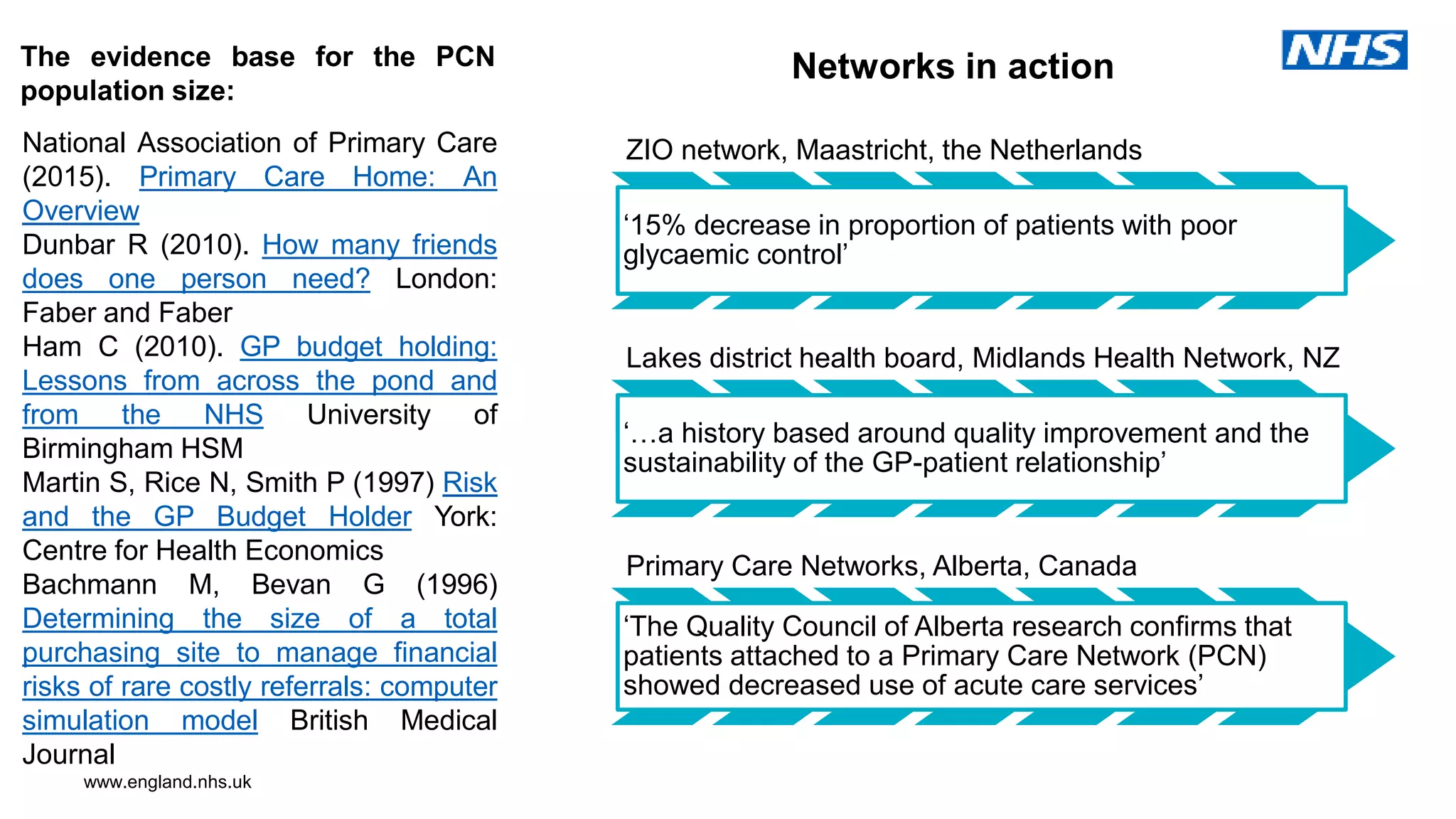
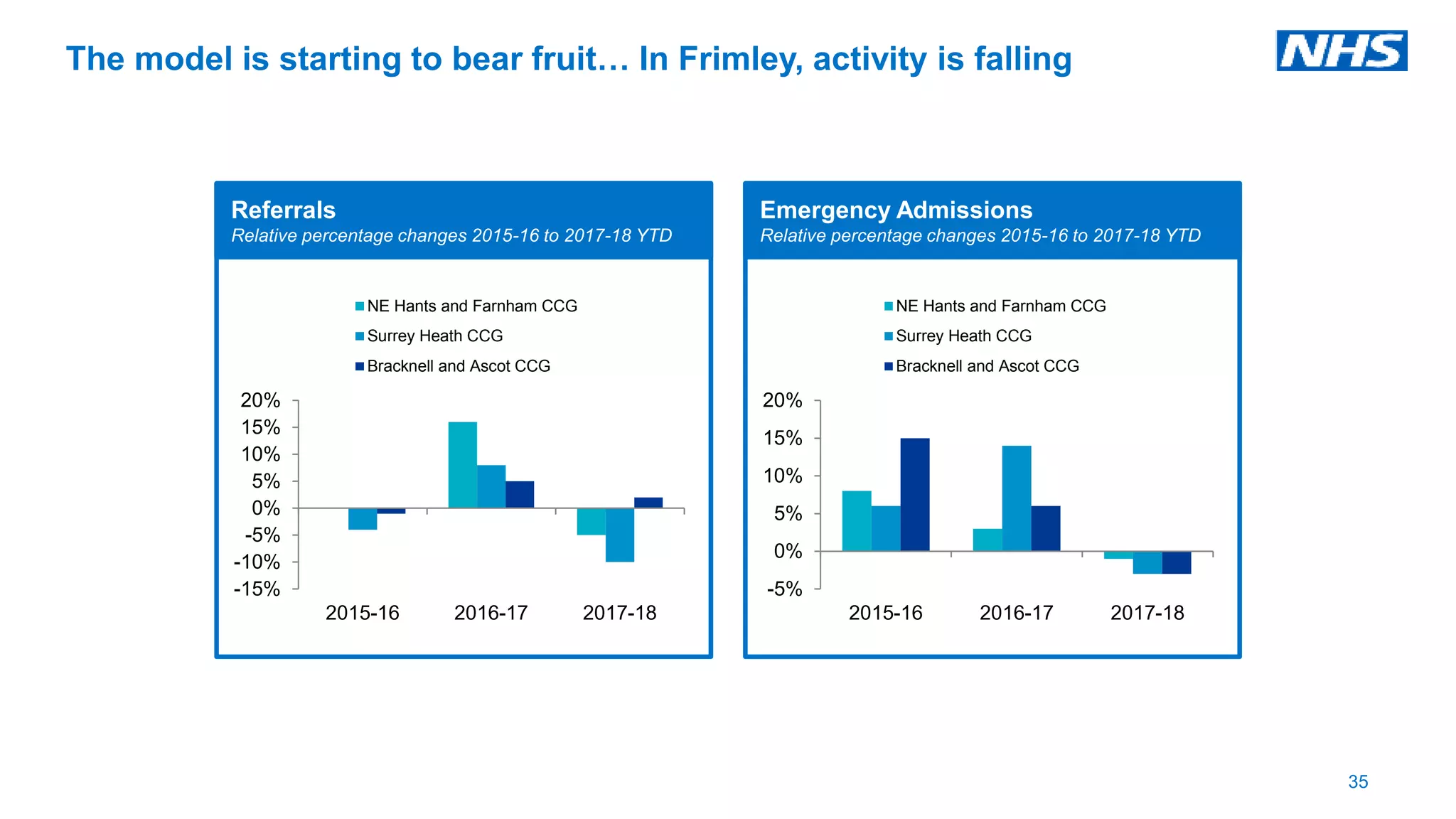
3) Early results show the new models are starting to have an impact, with a 15% reduction in referrals and emergency admissions in one integrated care