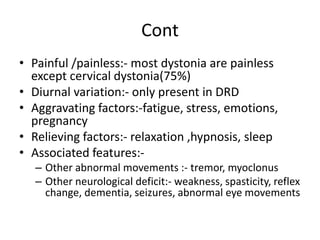
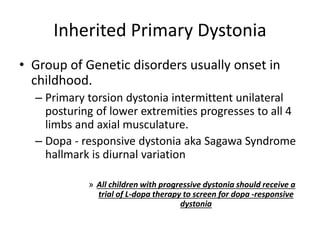
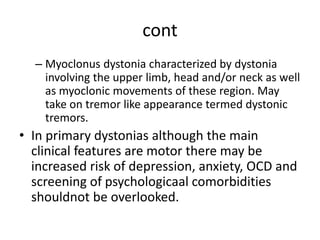
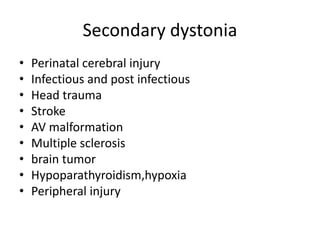
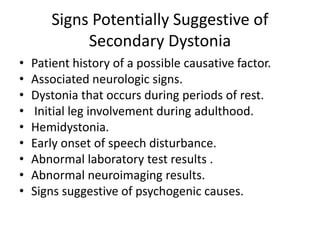
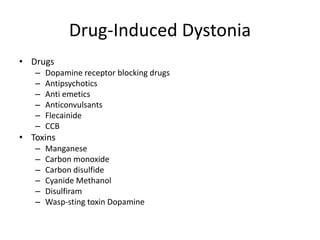
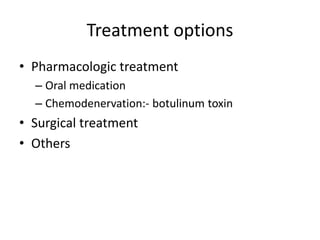
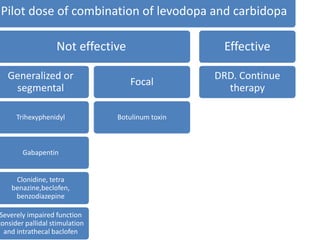
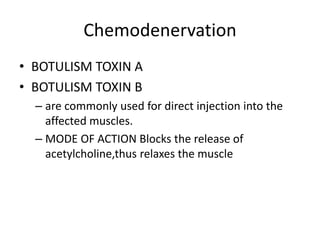
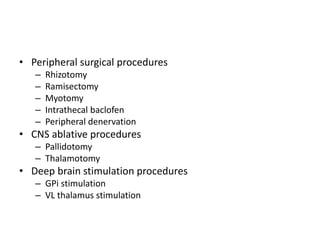
Dystonia is a neurological movement disorder characterized by sustained muscle contractions causing abnormal twisting movements or postures. It has several subtypes classified by anatomical distribution, age of onset, or etiology. Primary dystonia is genetic while secondary dystonia can be caused by injury, drugs, infections, or other neurological conditions. Symptoms vary but commonly involve twisting motions and abnormal postures. Treatment involves oral medications, botulinum toxin injections, surgery such as deep brain stimulation, or other therapies depending on the severity and type of dystonia.