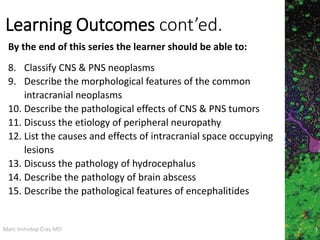
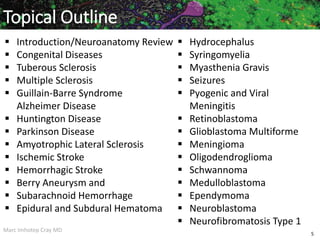
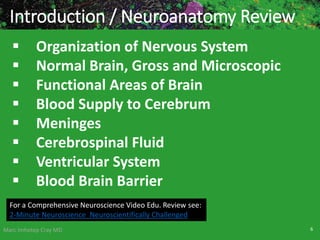
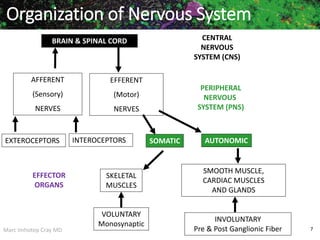
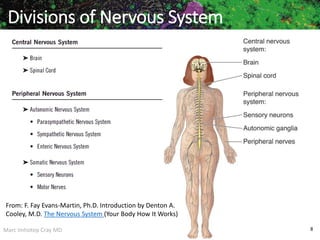
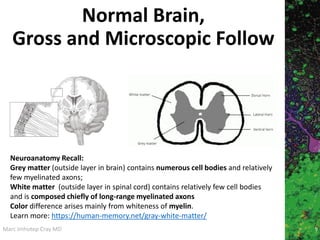
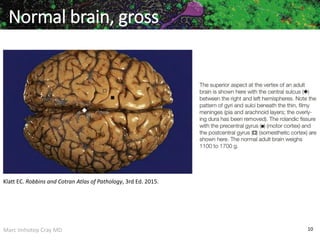
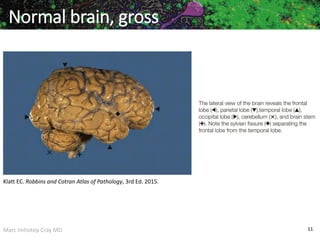
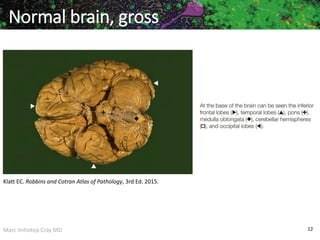
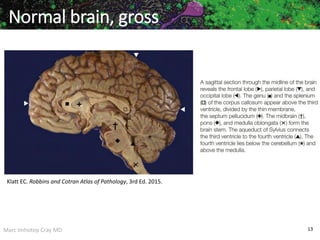
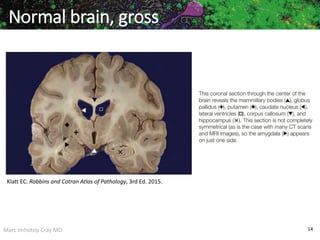
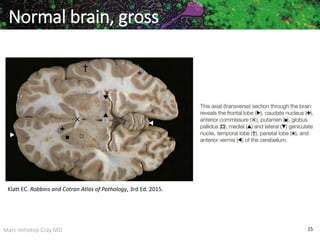
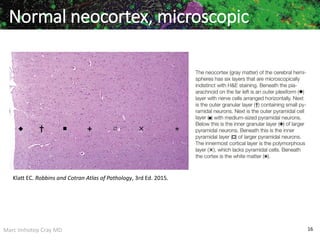
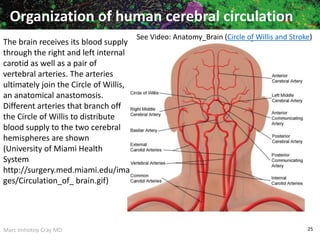
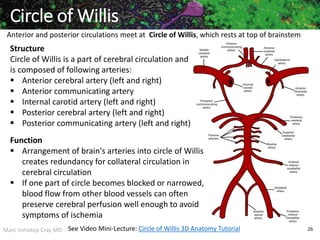
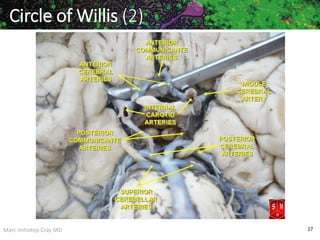
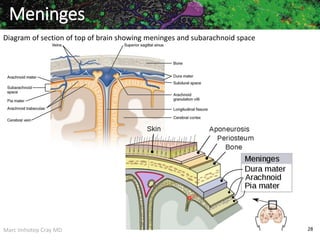
The document provides an overview of nervous system pathology presented by Marc Imhotep Cray, M.D. It outlines learning objectives related to describing various neurological disorders and diseases. It then covers topics like congenital diseases, multiple sclerosis, Alzheimer's disease, and various tumors of the central and peripheral nervous systems. Anatomical structures like the brain, ventricles, blood supply, and meninges are also reviewed at both the gross and microscopic level.


![Marc Imhotep Cray MD
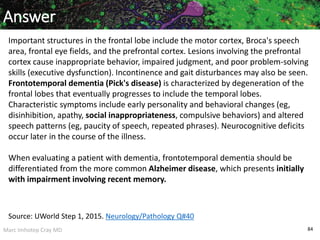
Basal Nuclei (Ganglia)
71
Components
Caudate nucleus
Putamen
Globus pallidus
Grouping of the Basal Nuclei (Ganglia)
The striatum consists of caudate nucleus and putamen
The lentiform nucleus consists of globus pallidus and
putamen
The corpus striatum consists of lentiform nucleus and
caudate nucleus
NB: Basal Nuclei The term basal ganglia is a misnomer. The cells forming
these structures are not “ganglia”—a term reserved to describe aggregations
of neuronal cell bodies[somata] (groups of nerve cell bodies ) in the peripheral
nervous system—but “nuclei” in the central nervous system.](https://image.slidesharecdn.com/nervoussystempathologyacase-basedlearningapproach-200806013443/85/Nervous-System-Pathology_A-Case-based-Learning-Approach-71-320.jpg)

![Marc Imhotep Cray MD
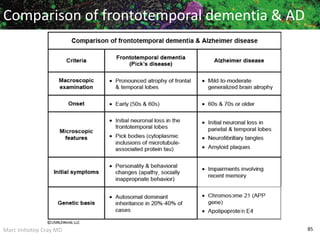
Multiple Sclerosis (2)
106
Clinical Manifestations: Relapsing and remitting course,
but eventually remissions become incomplete;
classic Charcot triad: nystagmus, scanning speech, and intention
tremor;
motor and sensory impairment of trunk and extremities
(hemiparesis, ataxia);
visual impairment (optic neuritis, retrobulbar neuritis,
internuclear ophthalmoplegia [on lateral gaze, one eye does not
adduct and abducting eye has nystagmus caused by demyelination
of MLF]); urinary/bowel incontinence owing to loss of sphincter
control
Lab findings: Lumbar puncture shows mild lymphocytosis and
elevated IgG, manifested as multiple oligoclonal bands on
electrophoresis
Treatment: Corticosteroids and other immunosuppressants](https://image.slidesharecdn.com/nervoussystempathologyacase-basedlearningapproach-200806013443/85/Nervous-System-Pathology_A-Case-based-Learning-Approach-106-320.jpg)
![Marc Imhotep Cray MD
Stroke (CVA) Capsule
CVA present clinically as sudden neurological
defects and may be caused by
intracranial hemorrhage (hemorrhagic stroke) (e.g.
subarachnoid or intracranial hemorrhage) or
cerebral infarction (usually secondary to thrombotic
[ischemic stroke] or embolic occlusion of a carotid or
intracranial artery) embolic stroke
Strokes may lead to death or permanent severe
neurological defects but modern therapies can
result in remarkable clinical recovery
118](https://image.slidesharecdn.com/nervoussystempathologyacase-basedlearningapproach-200806013443/85/Nervous-System-Pathology_A-Case-based-Learning-Approach-118-320.jpg)





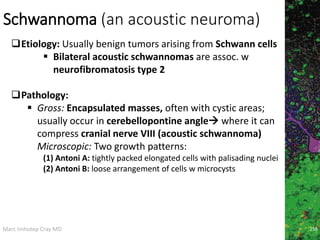
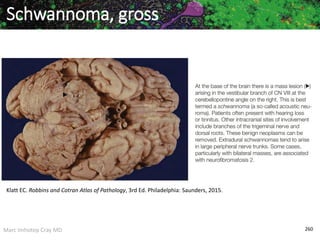
![Marc Imhotep Cray MD
Schwannoma (2)
259
Clinical Manifestations: Presents w Sx assoc. w
compression of involved nerve (cranial nerve VIII
compression leads to pts. presenting w ipsilateral
hearing loss, tinnitus, and vertigo), seizures, headaches,
N/V, and other signs of increased ICP
Treatment and Prognosis:
Surgical resection of tumor
Prognosis is good
Note: Pineal tumors usually occur in young men betw. ages of 10 and 40
Presents w Parinaud syndrome (paralysis of upward gaze caused
by pre-tectal and superior colliculus damage,
Obstructive hydrocephalus [owing to compression of aqueduct of
Sylvius], and
Endocrine abnormalities [owing to compression of hypothalamus])](https://image.slidesharecdn.com/nervoussystempathologyacase-basedlearningapproach-200806013443/85/Nervous-System-Pathology_A-Case-based-Learning-Approach-259-320.jpg)