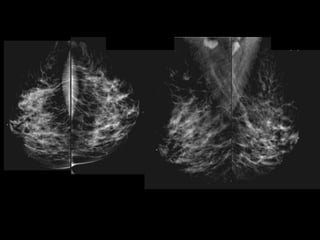
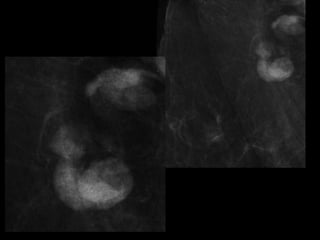
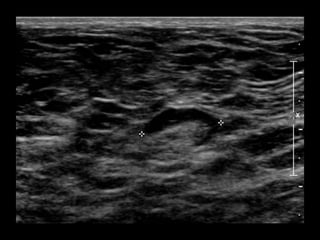
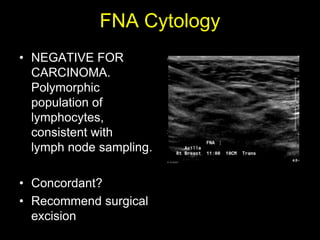
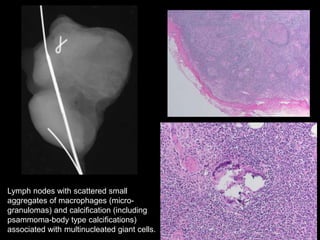
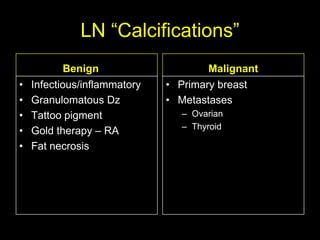
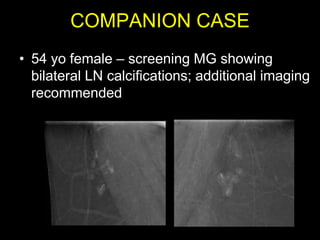
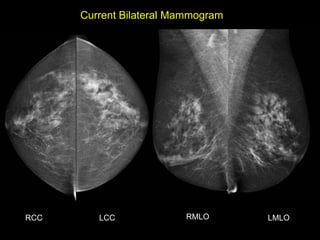
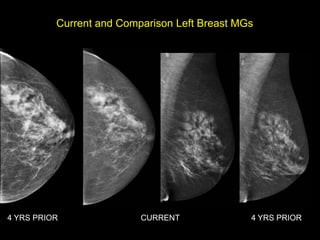
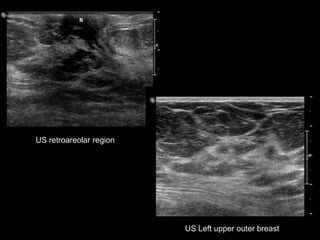
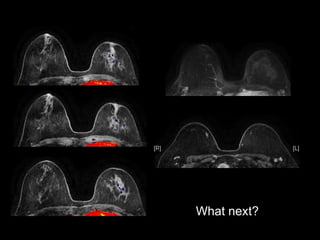
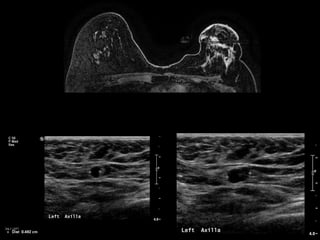
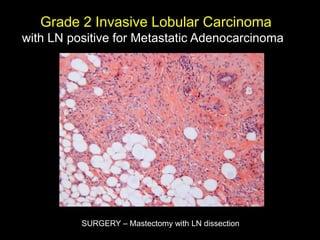
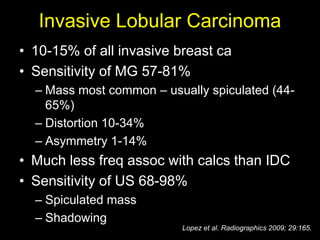
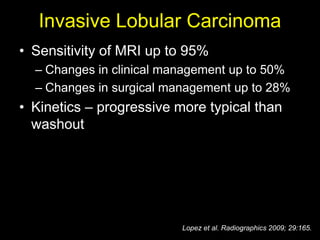
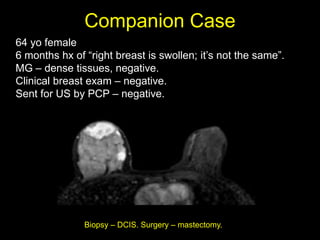
This document contains a panel of unknown cases presented by Dr. Tejas Mehta at NERRS: Women's Imaging on April 5, 2013. The first case involves a 61-year-old woman with a family history of breast and ovarian cancer who presented for routine screening mammography. The second case discusses the imaging and biopsy findings of a 54-year-old woman with bilateral lymph node calcifications found on screening mammography. The third case presents a 65-year-old woman with a left breast mass and nipple change, whose mammogram and ultrasound revealed a grade 2 invasive lobular carcinoma.