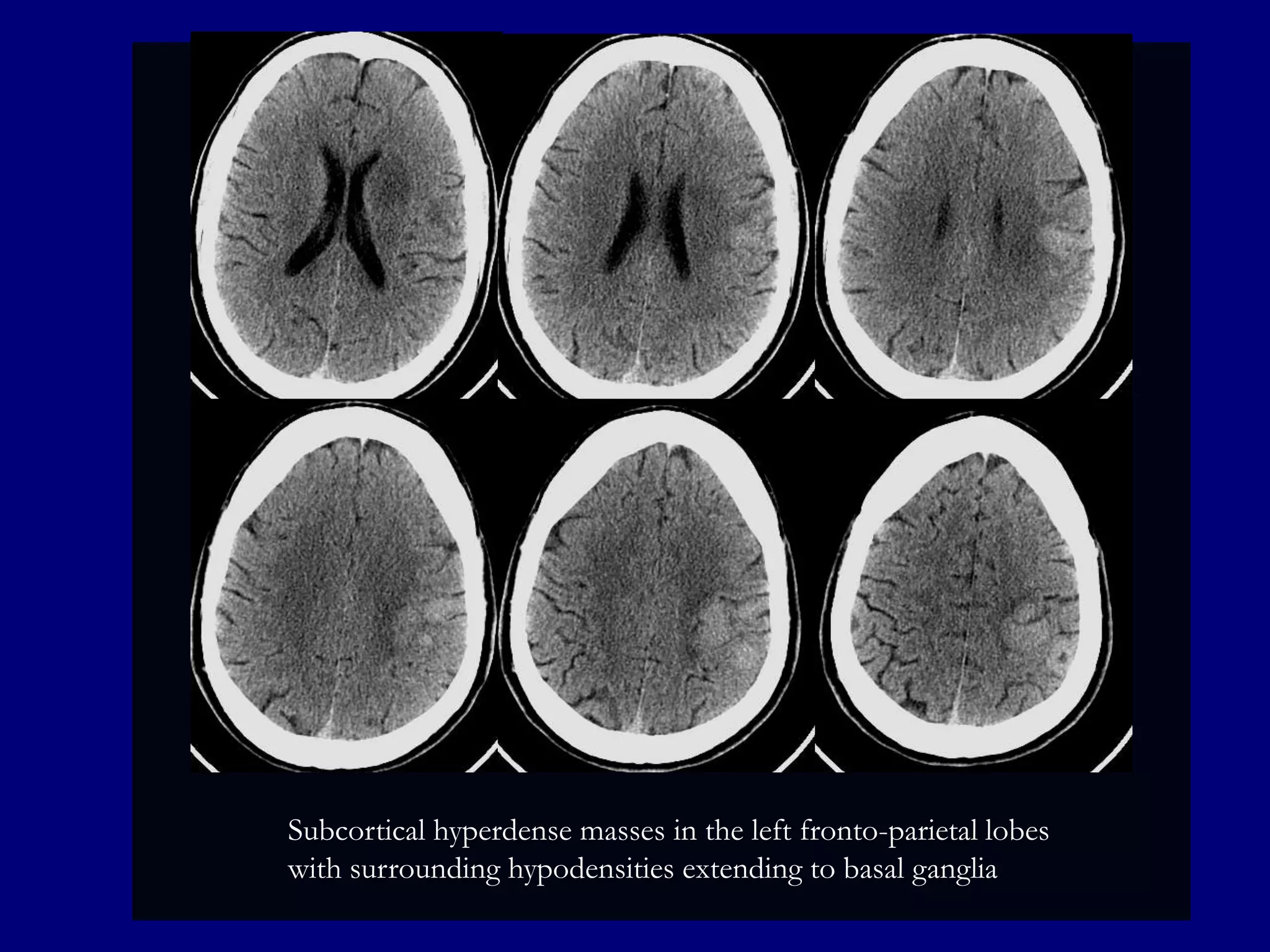
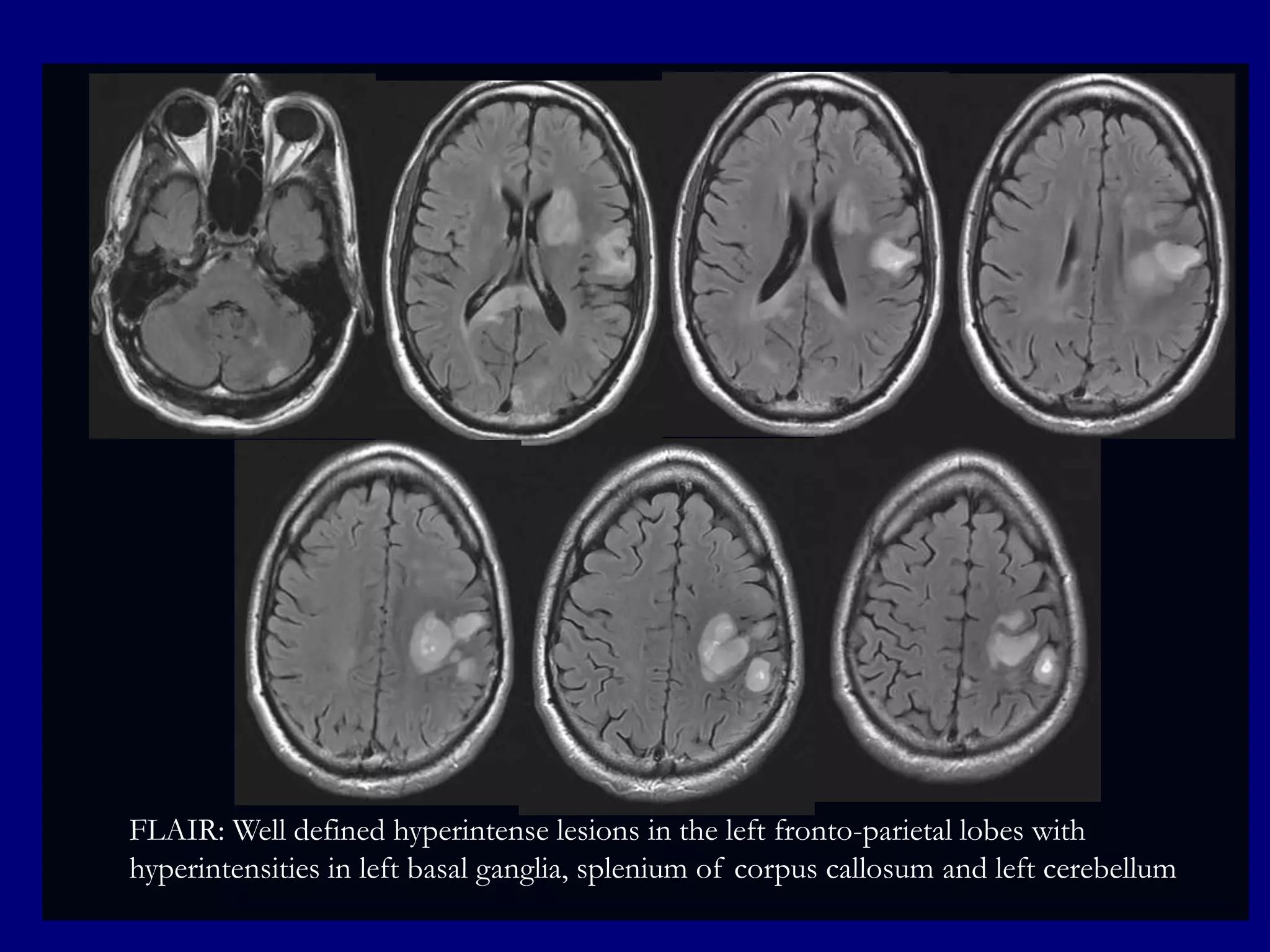
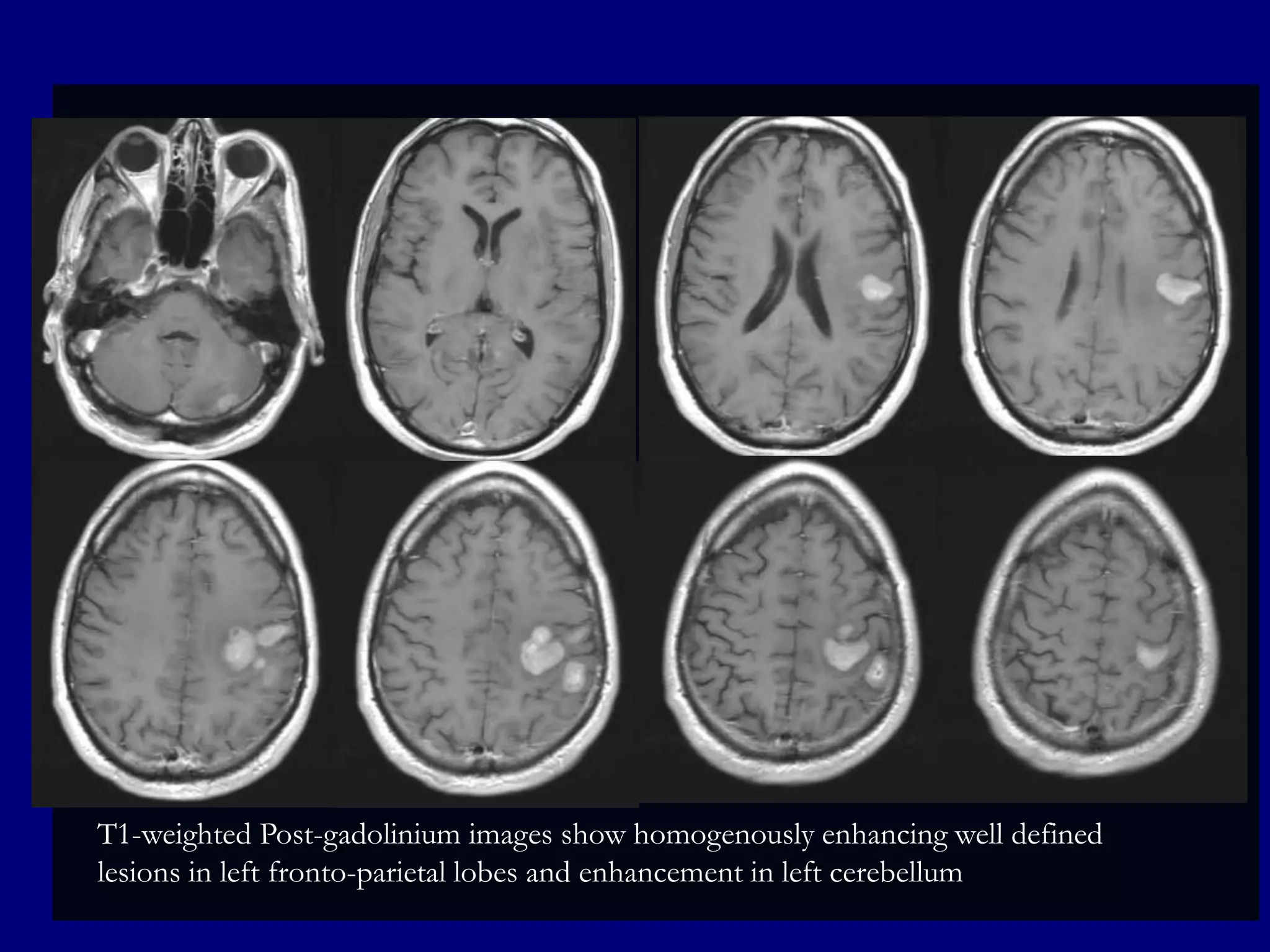
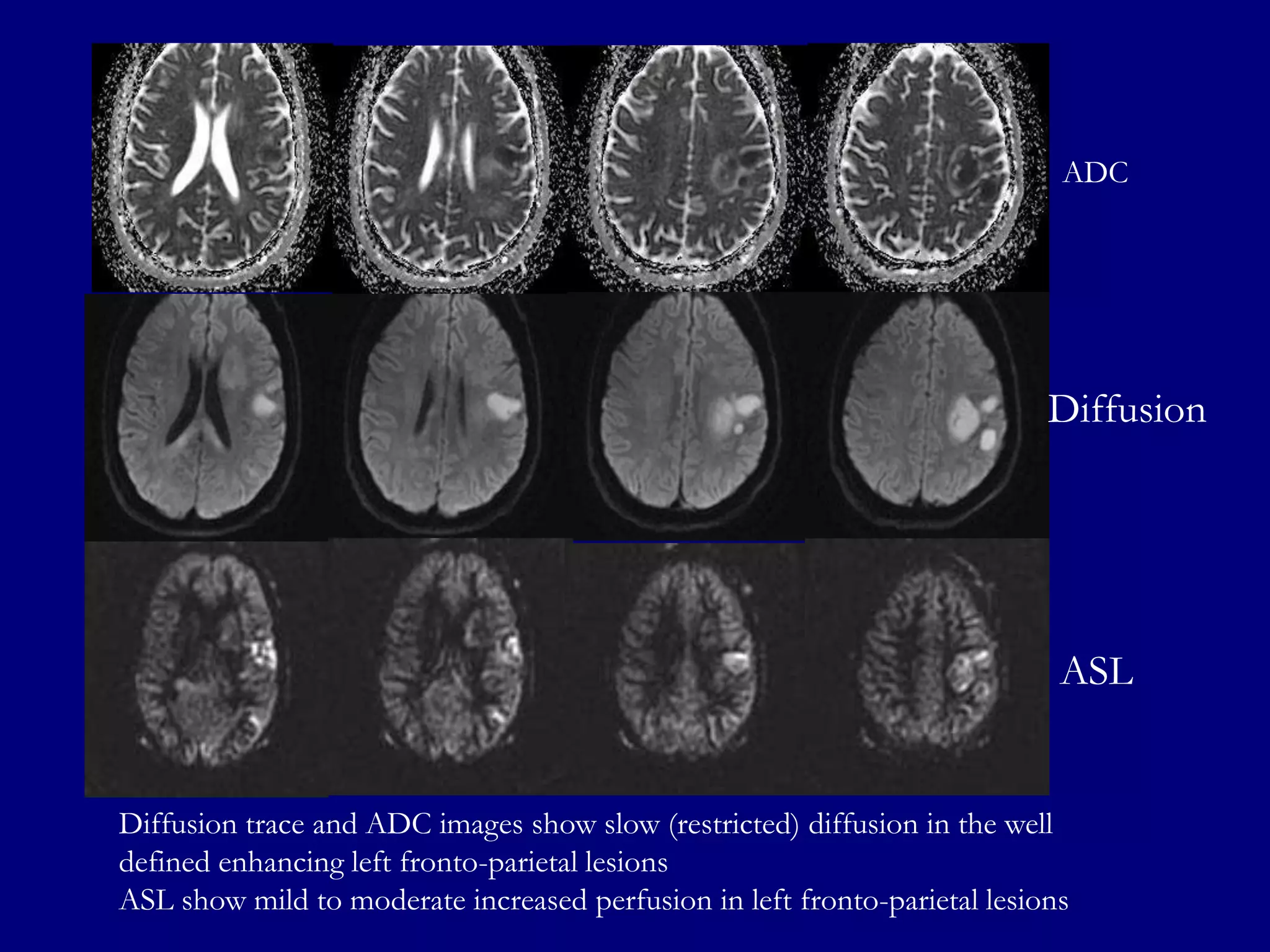
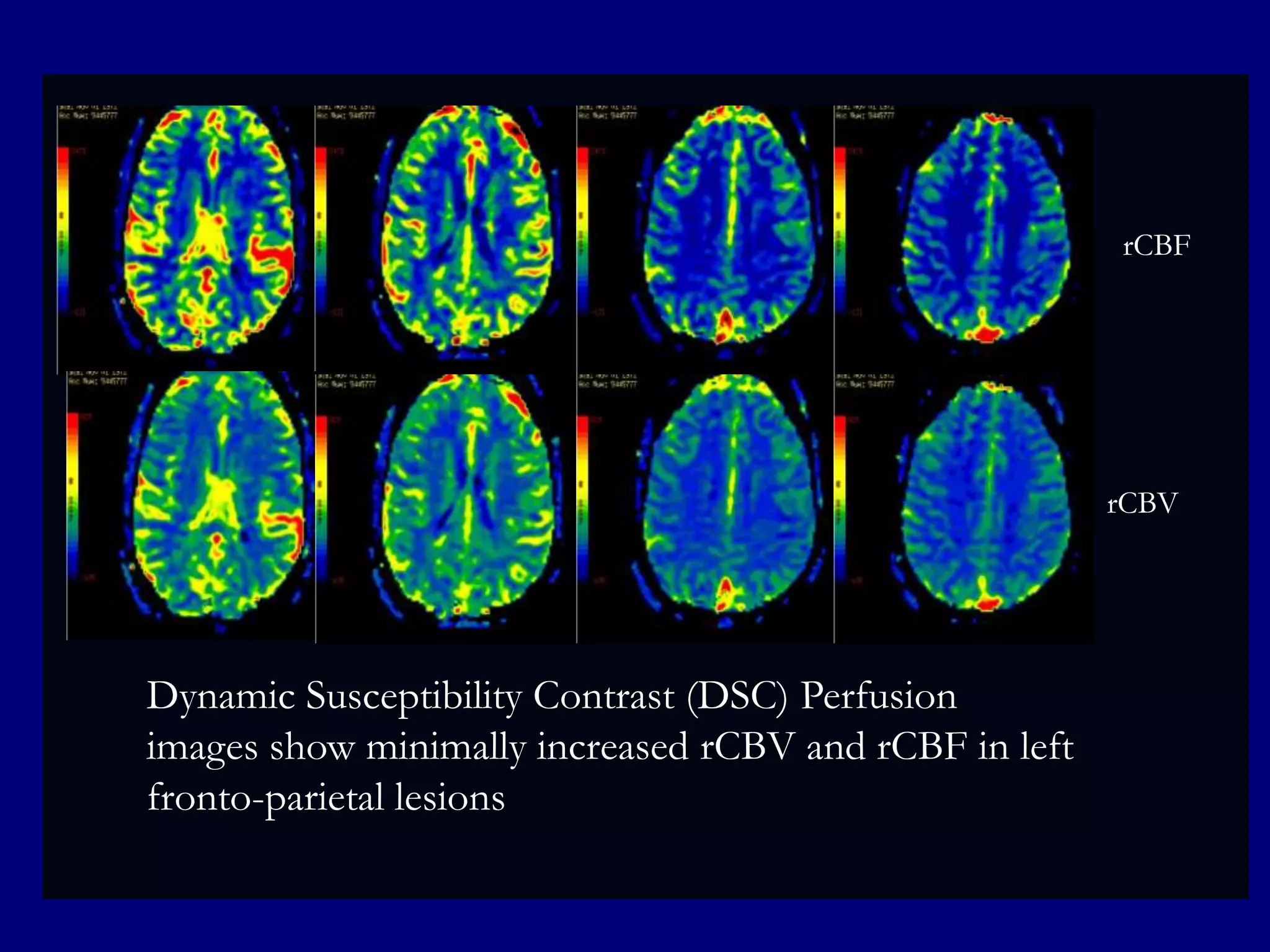
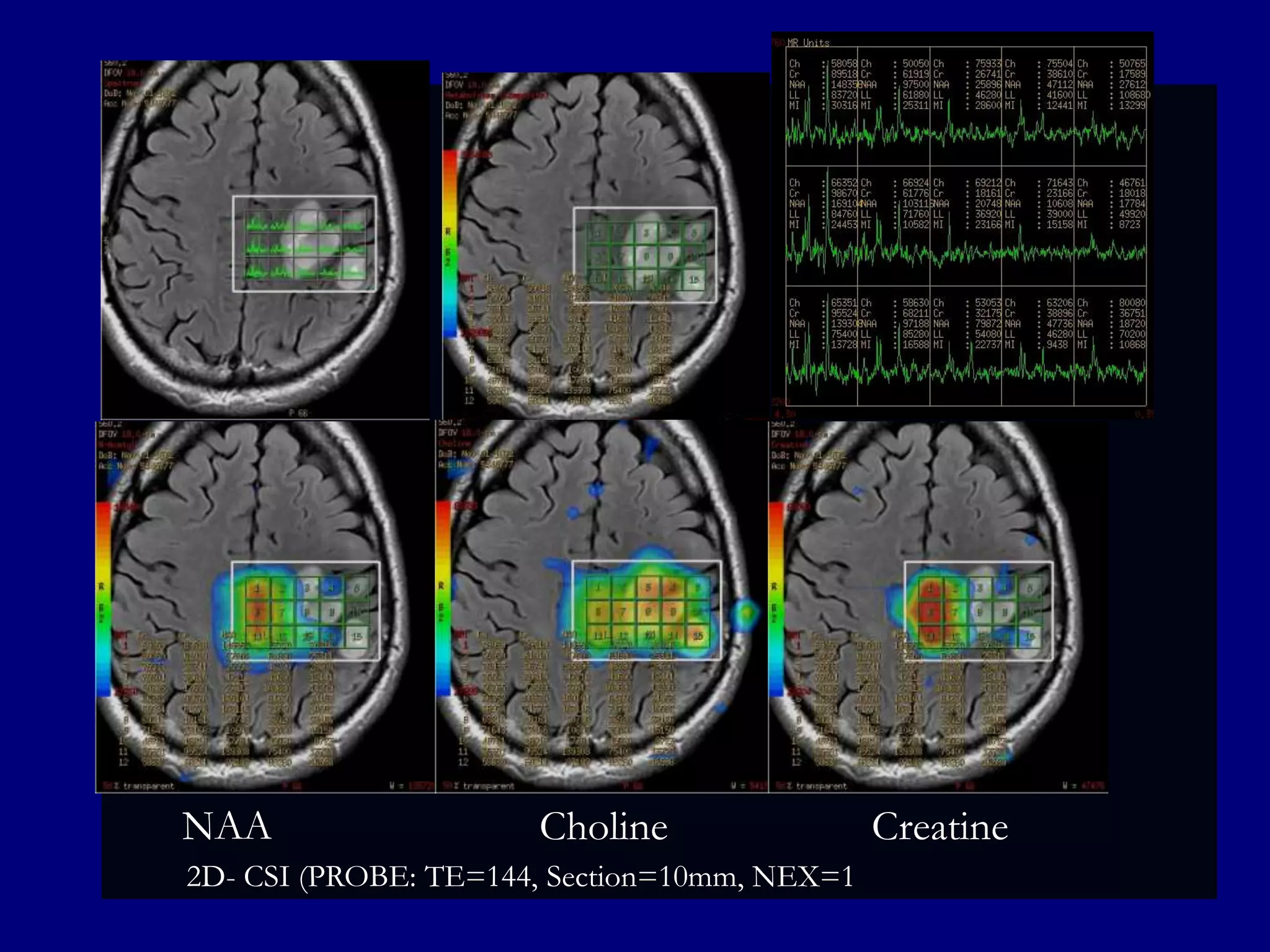
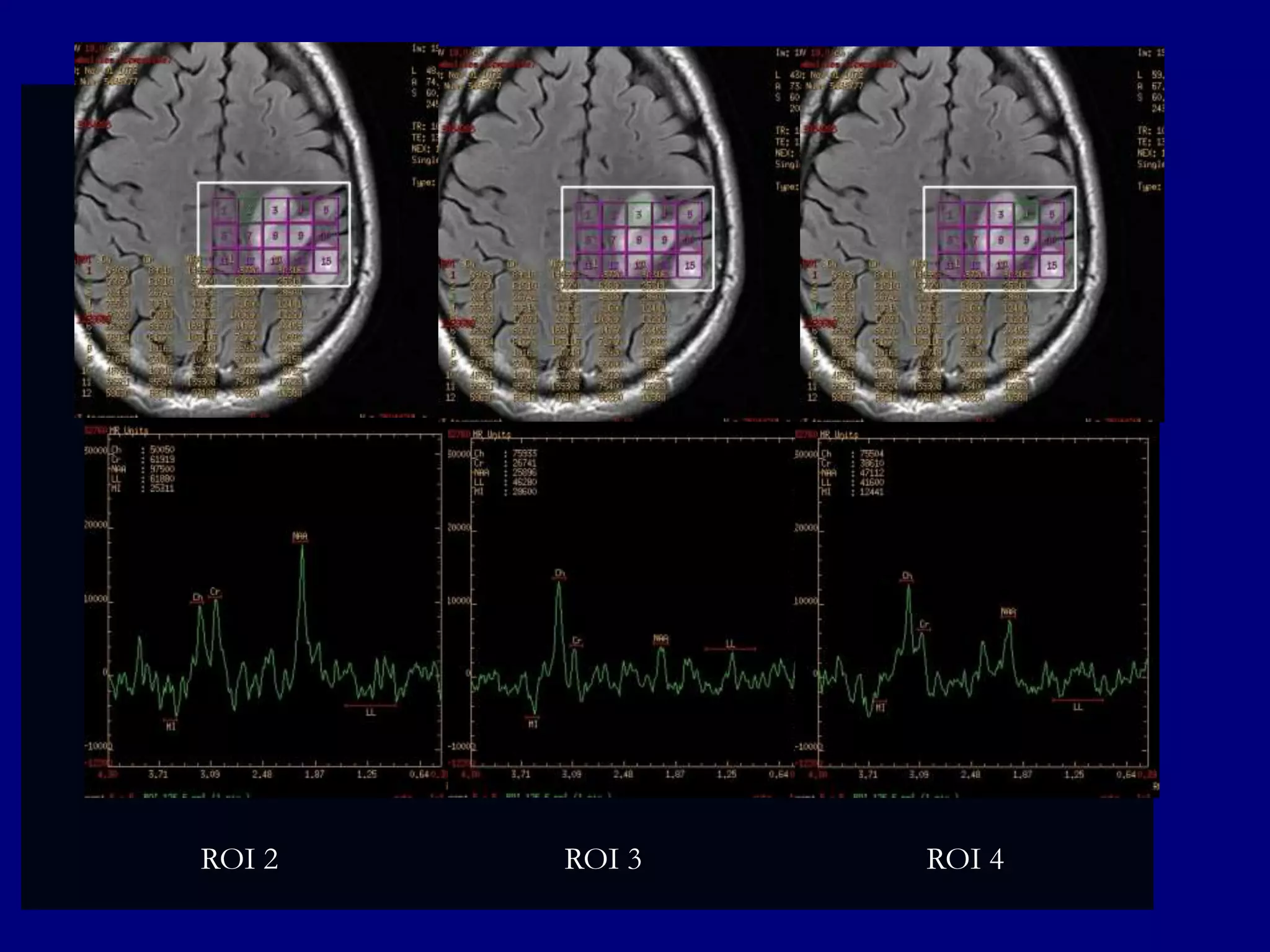
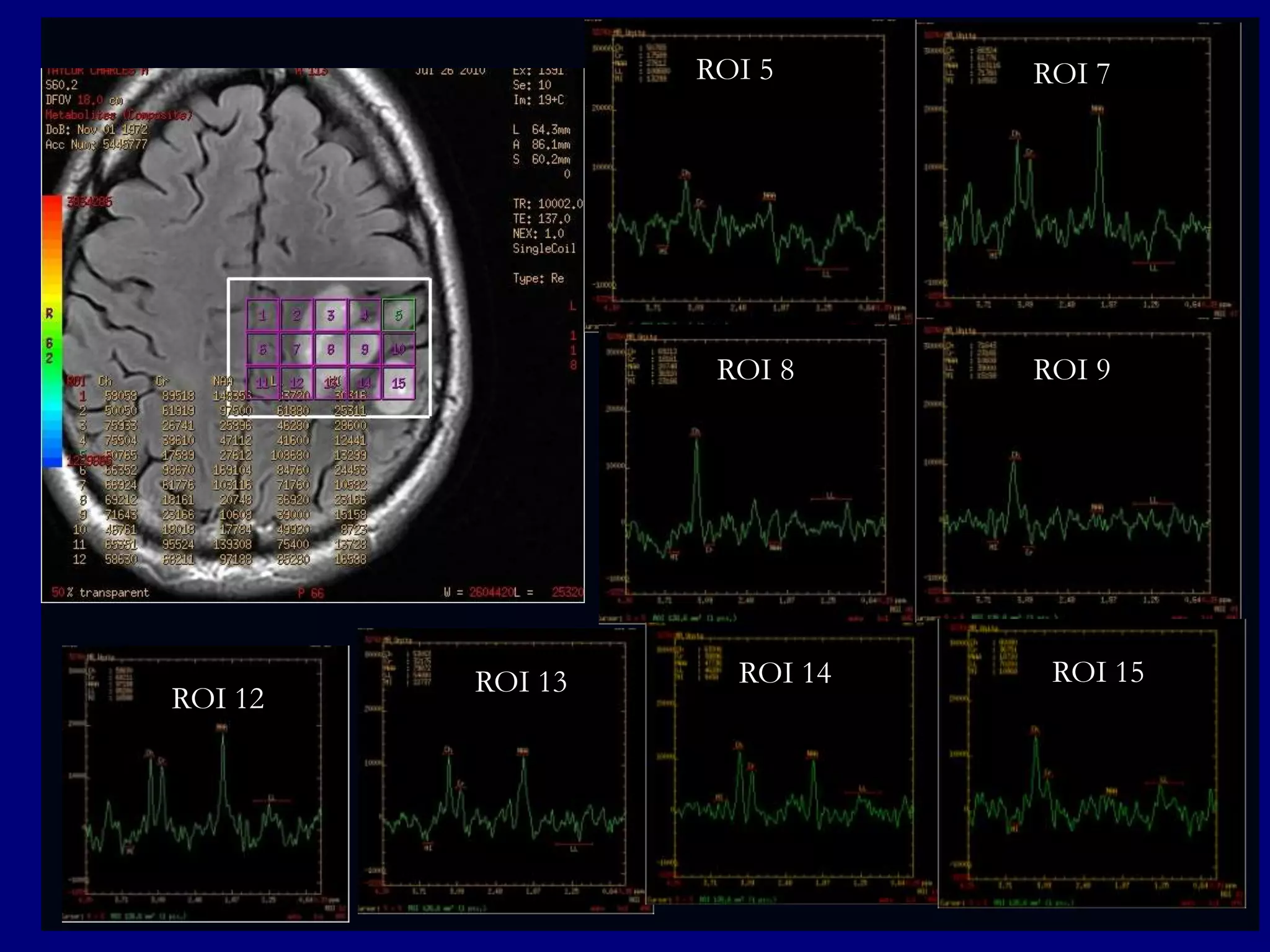
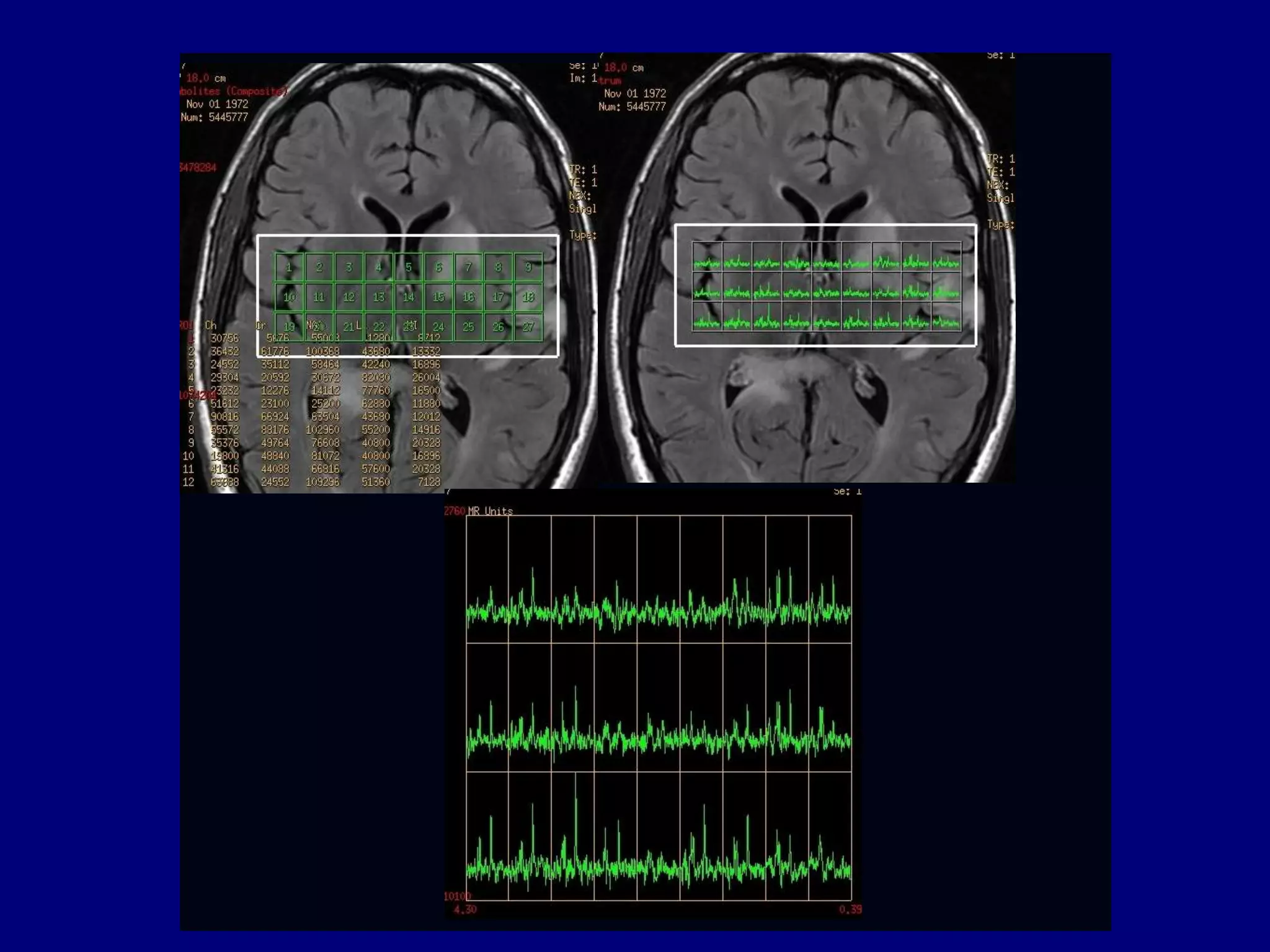
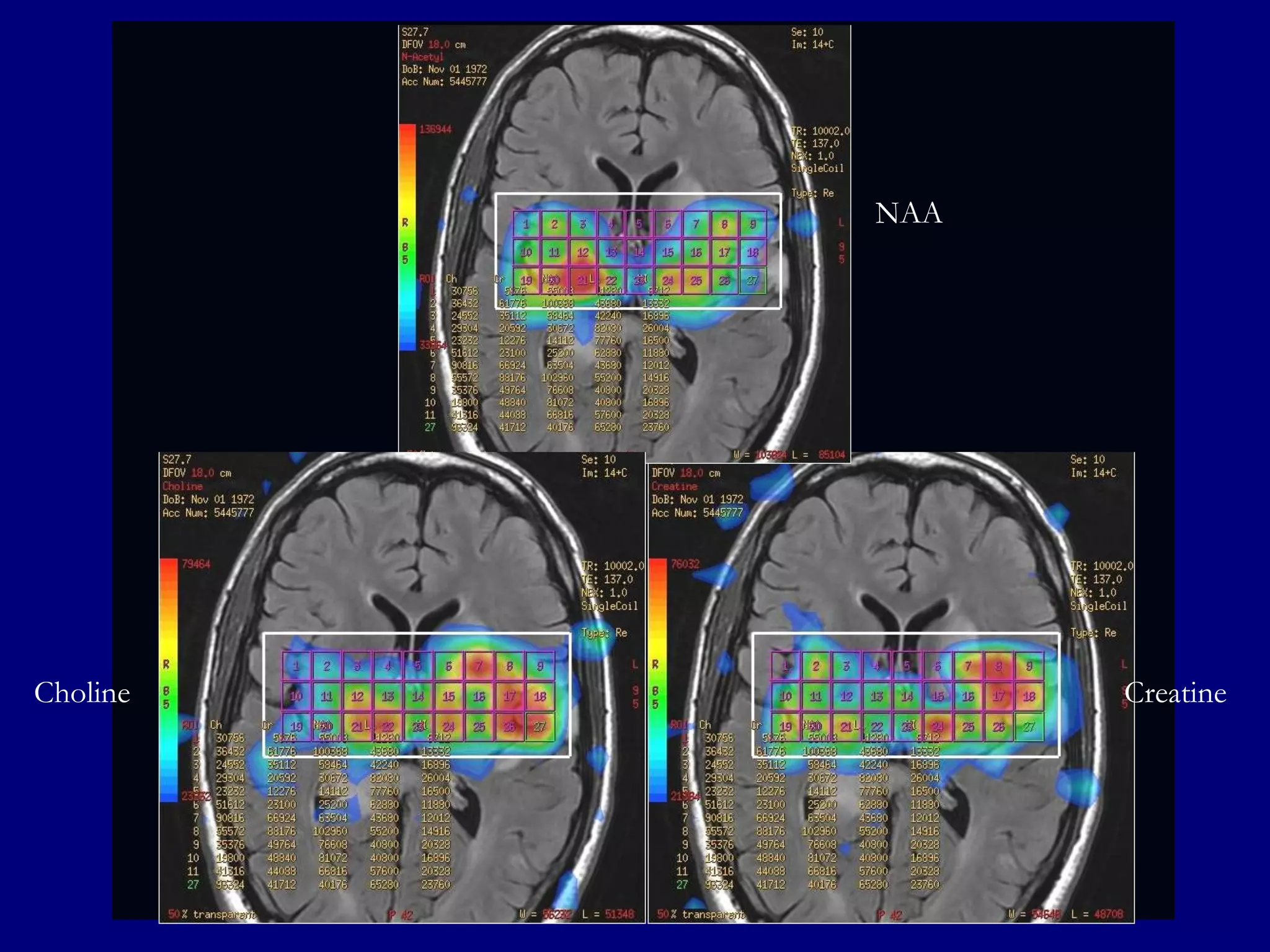
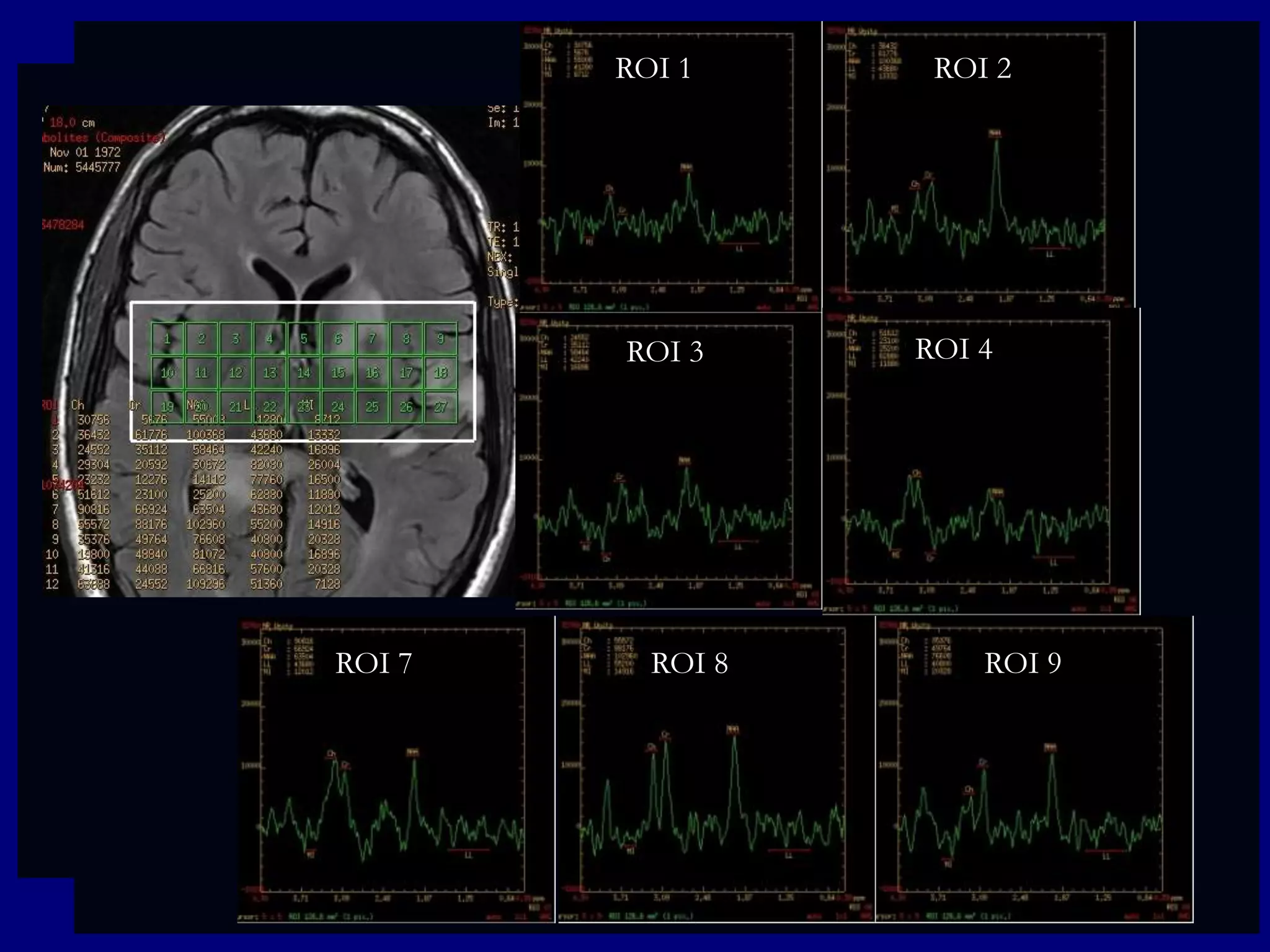
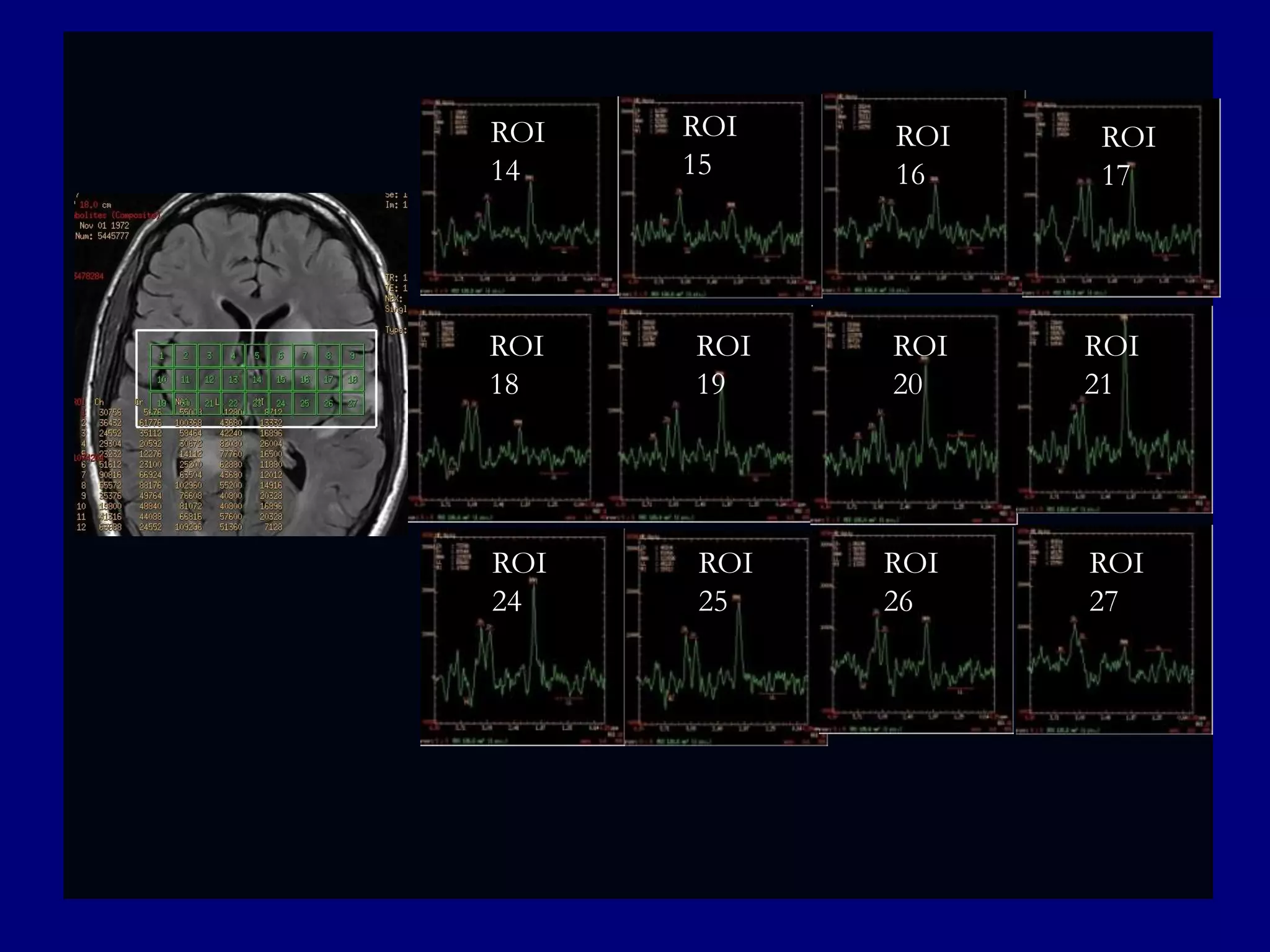
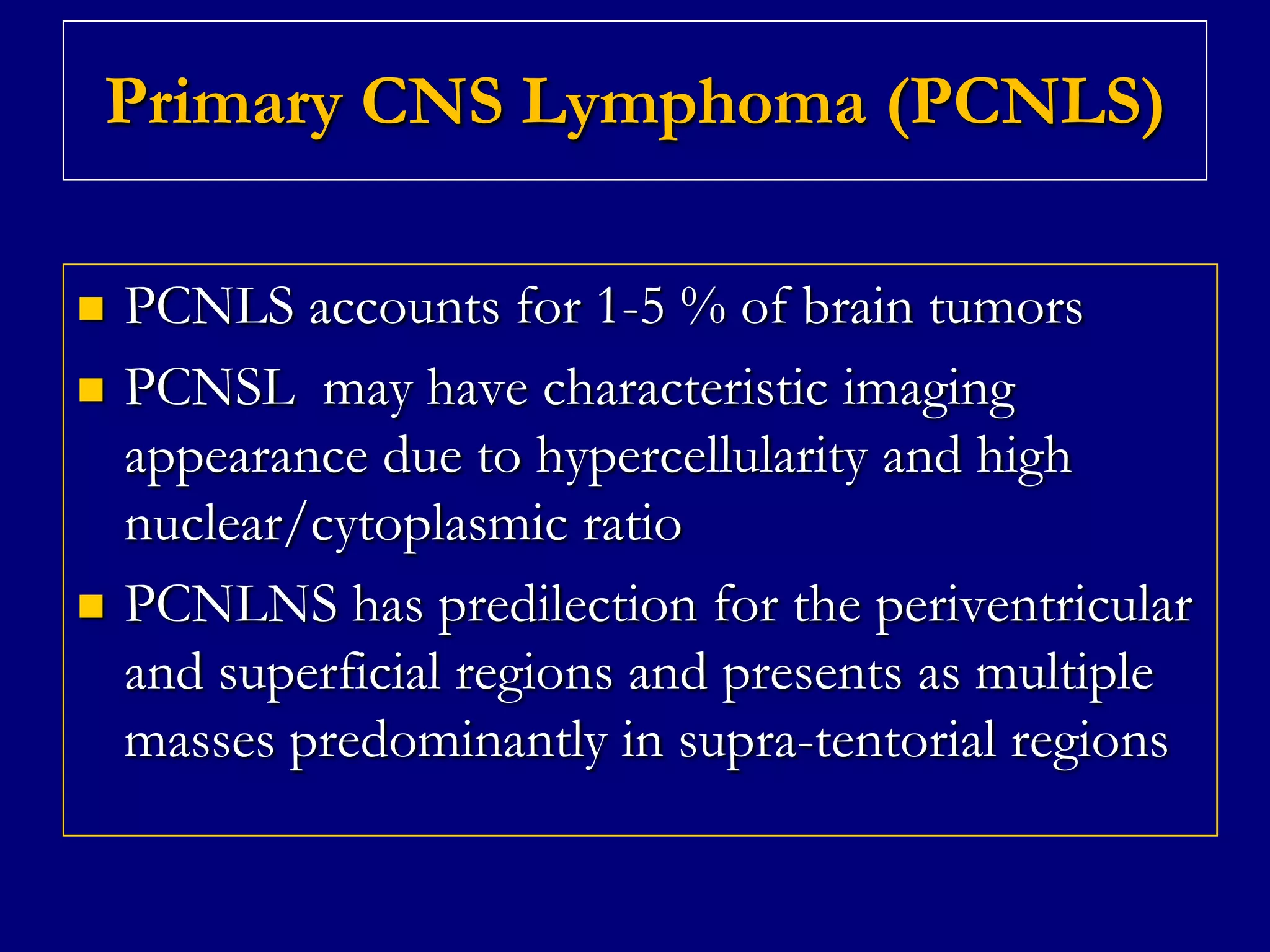
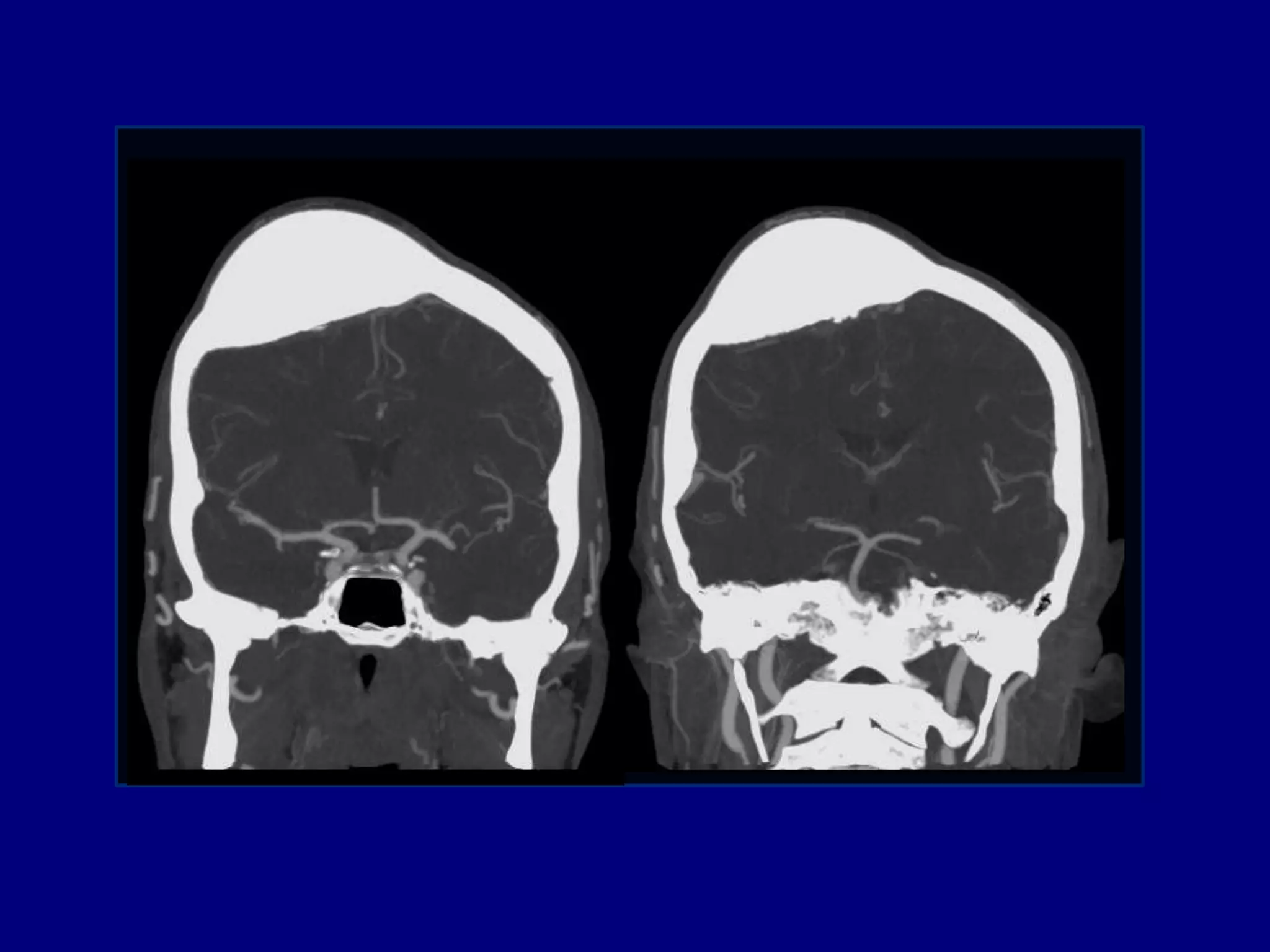
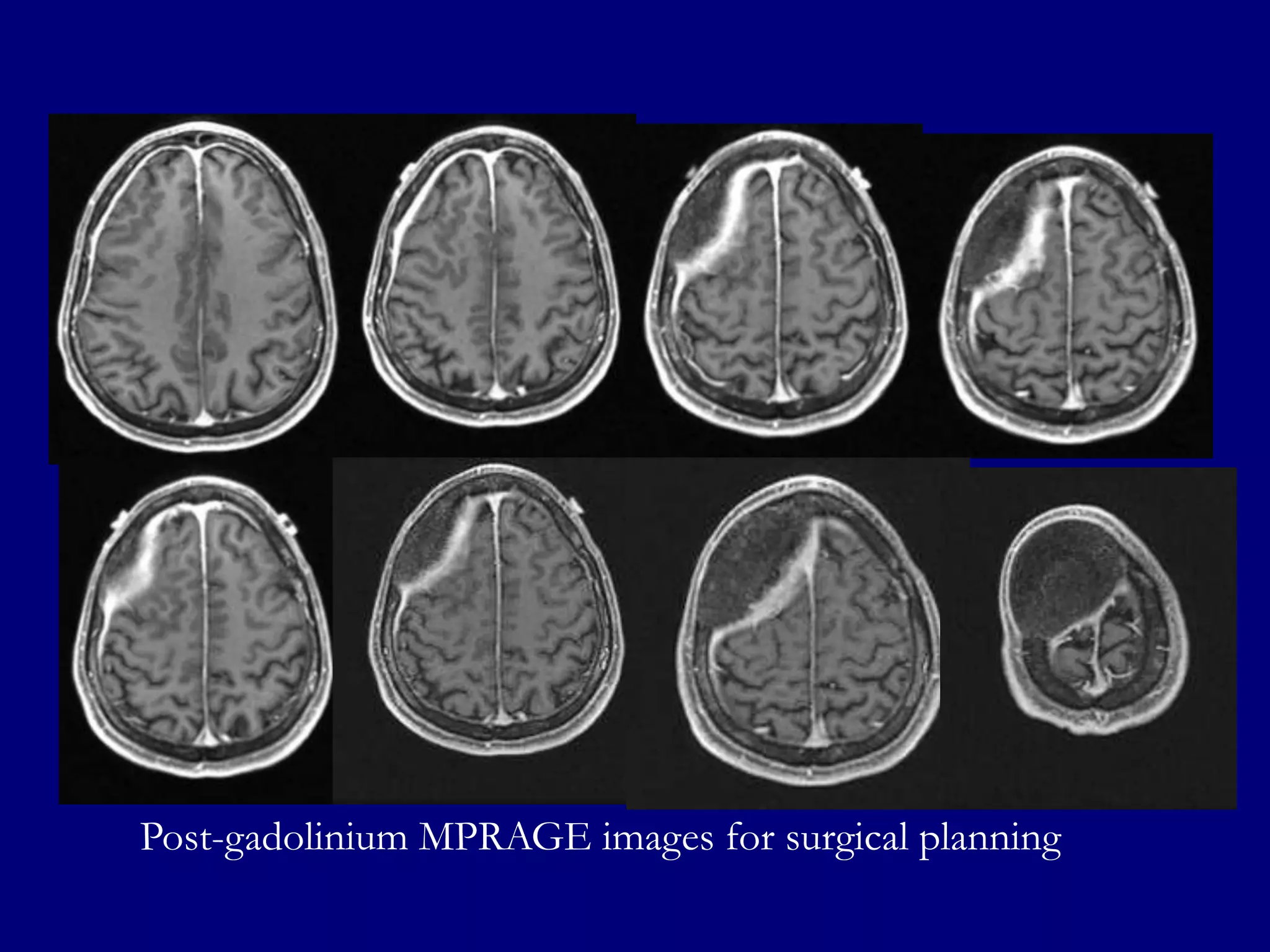
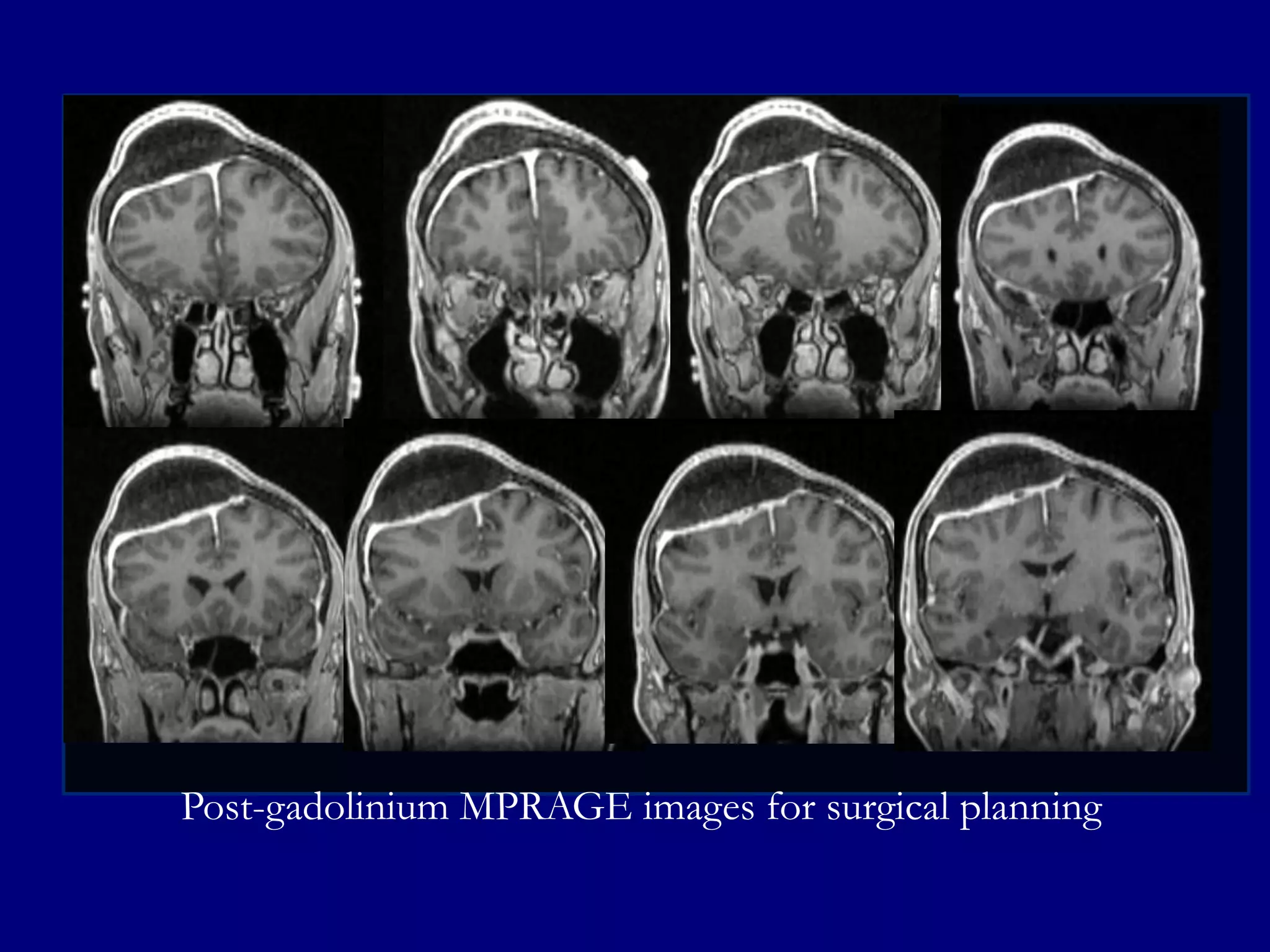
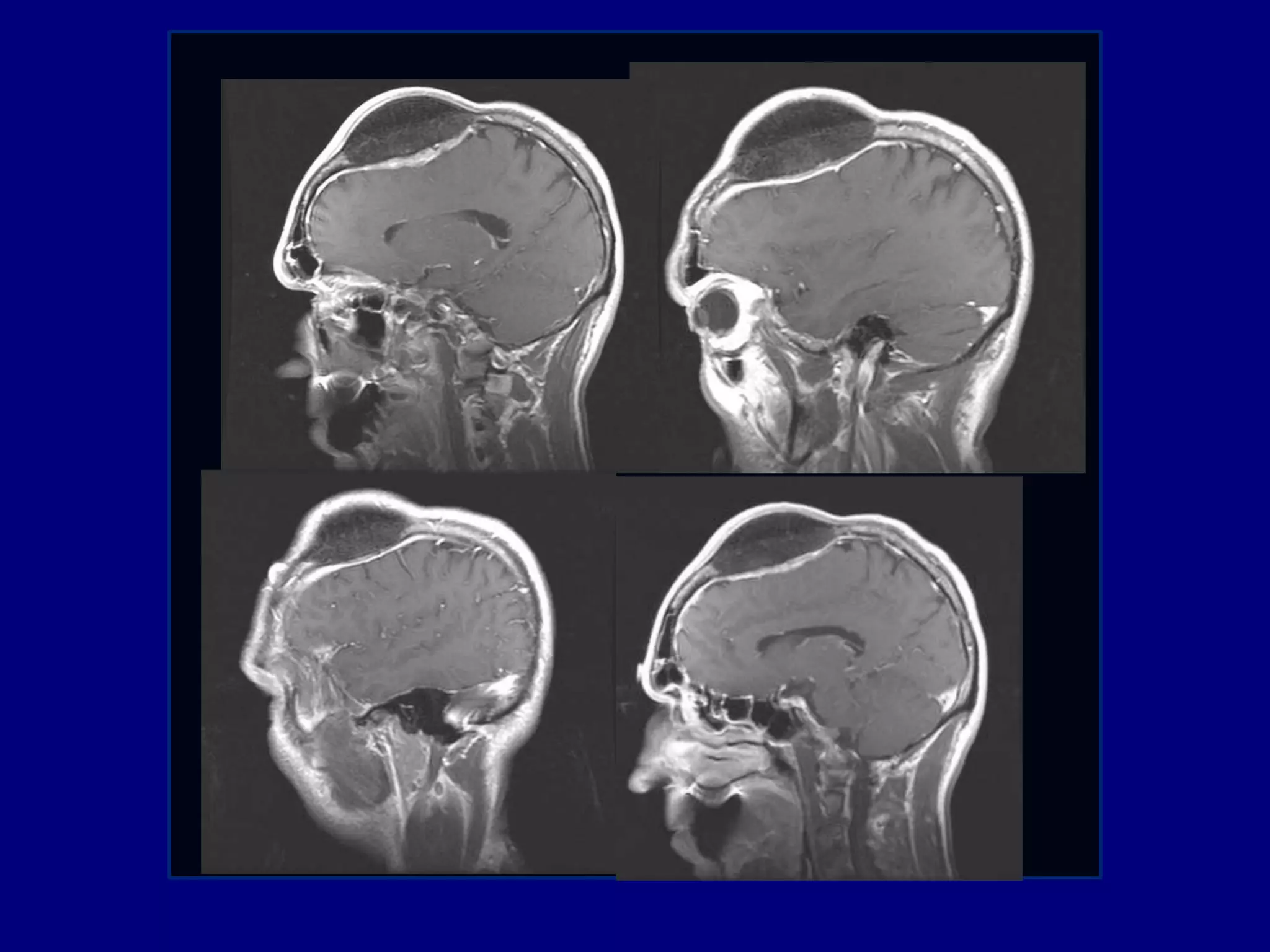
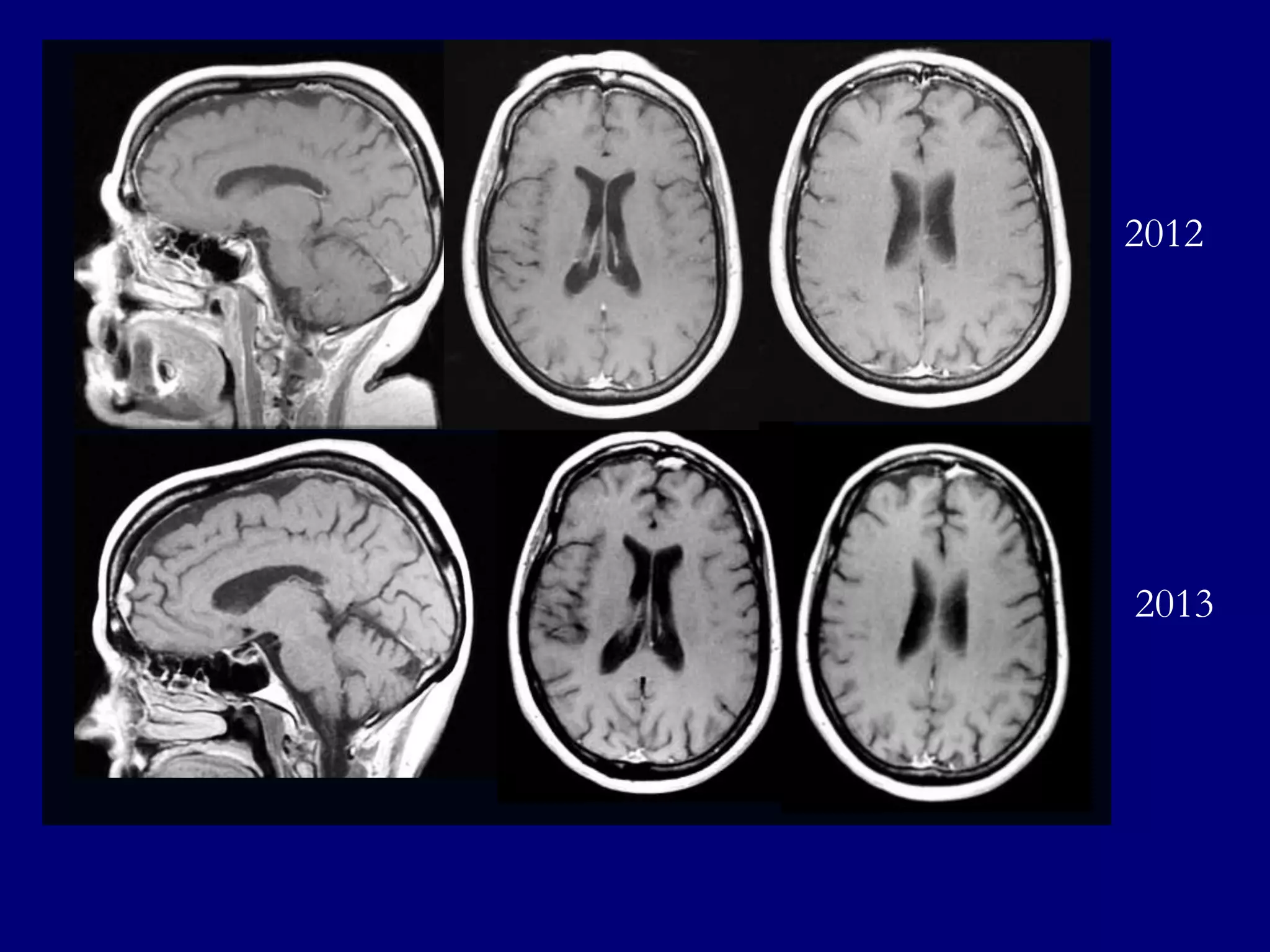
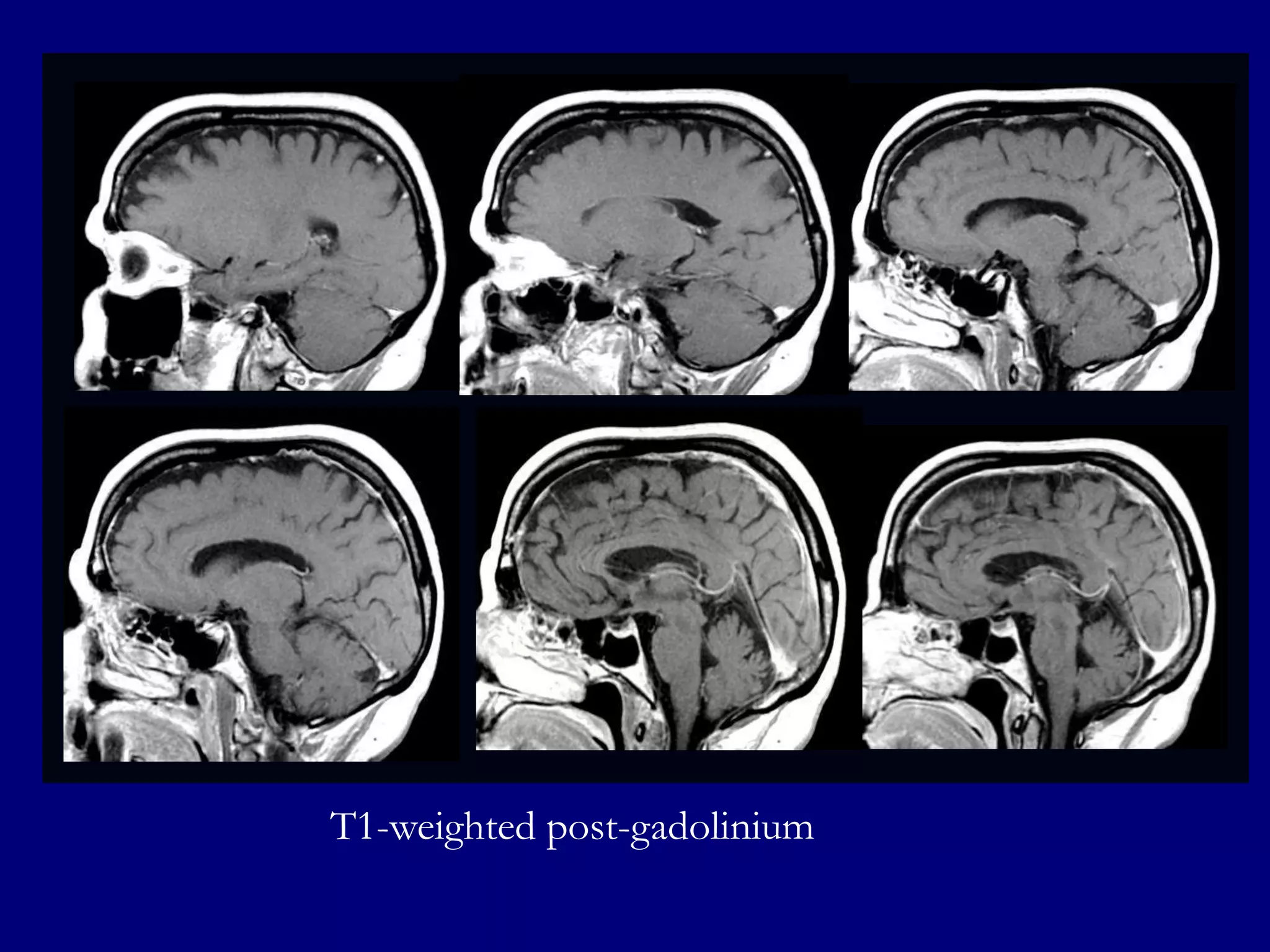
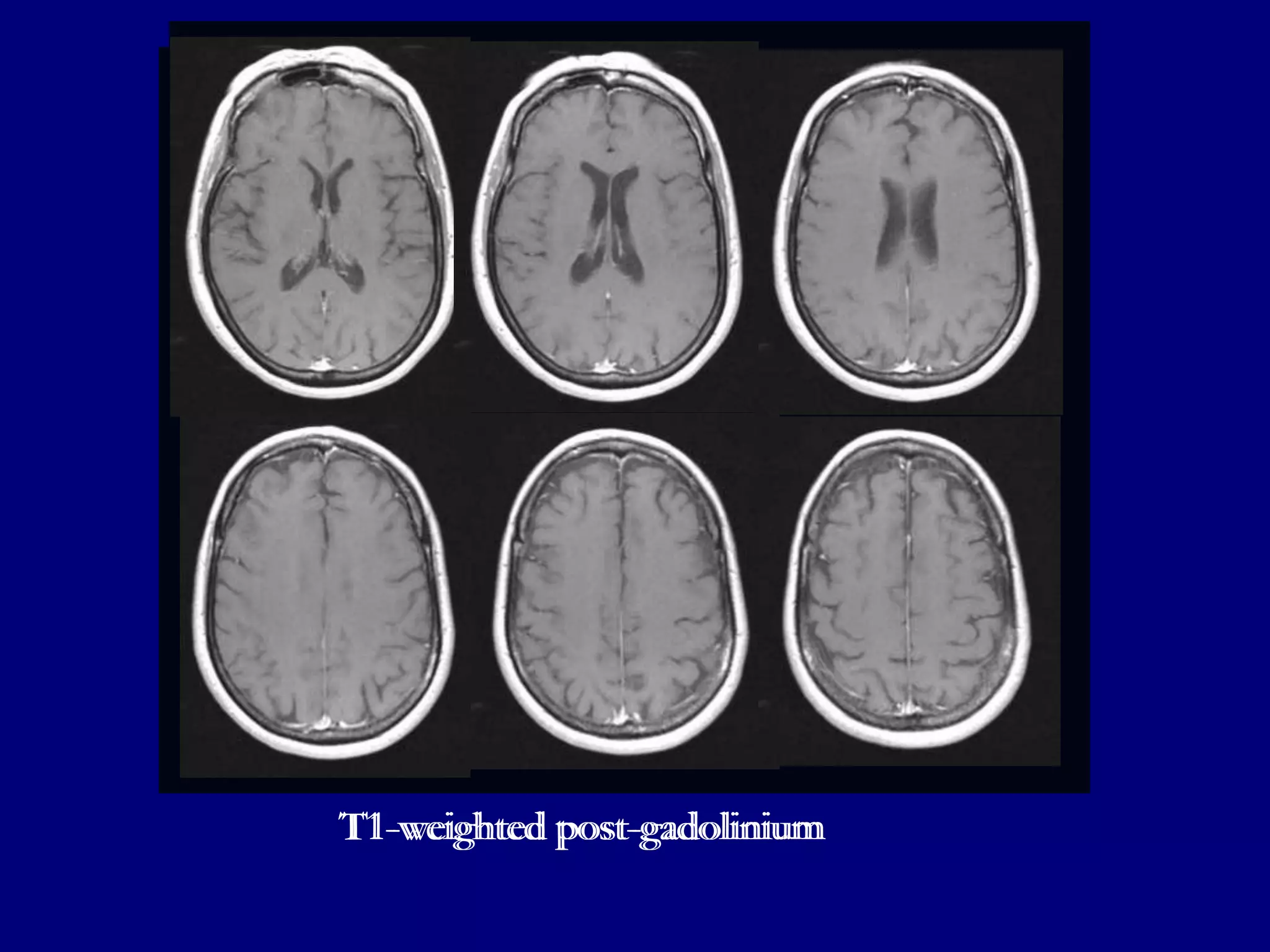
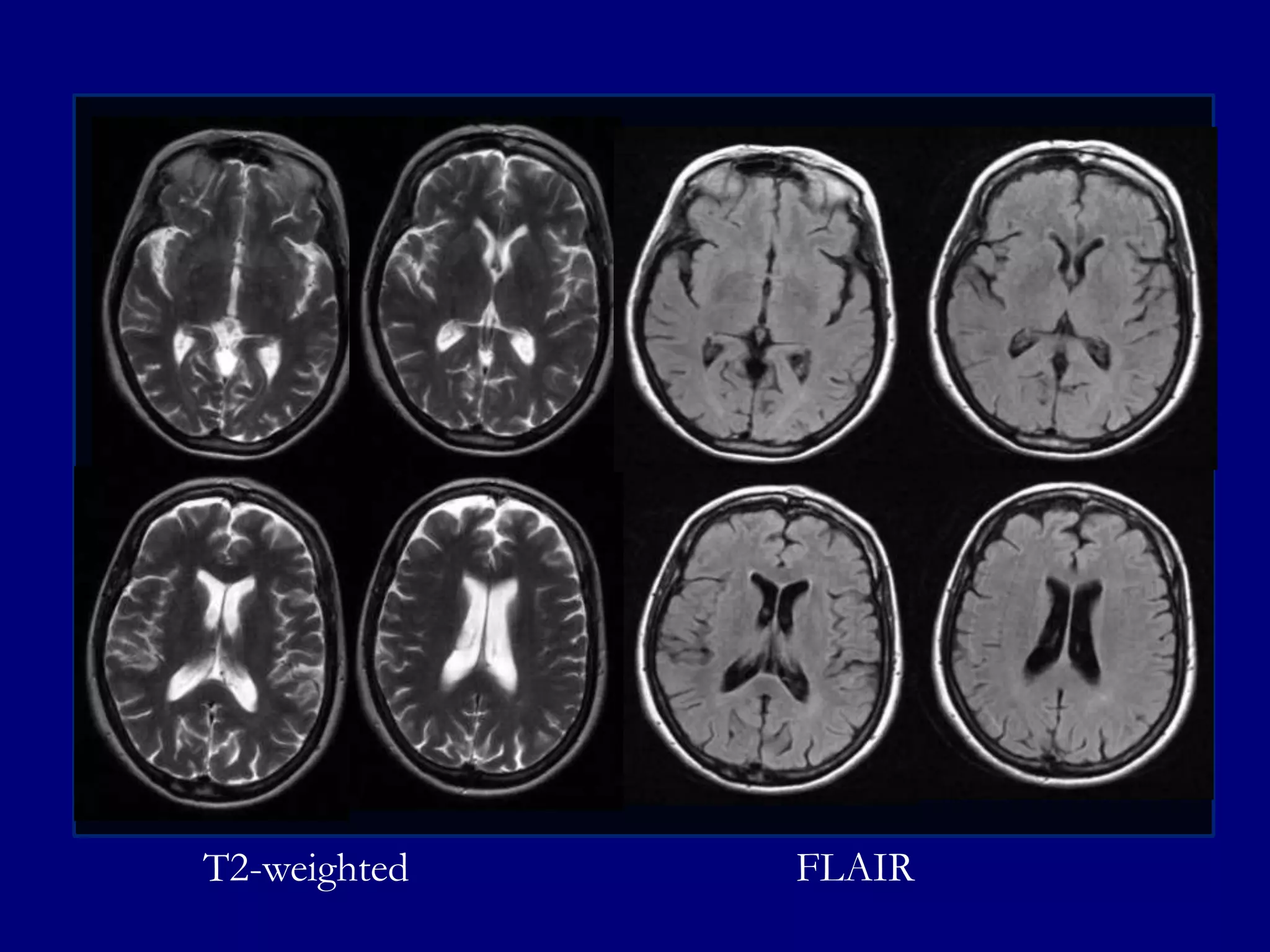
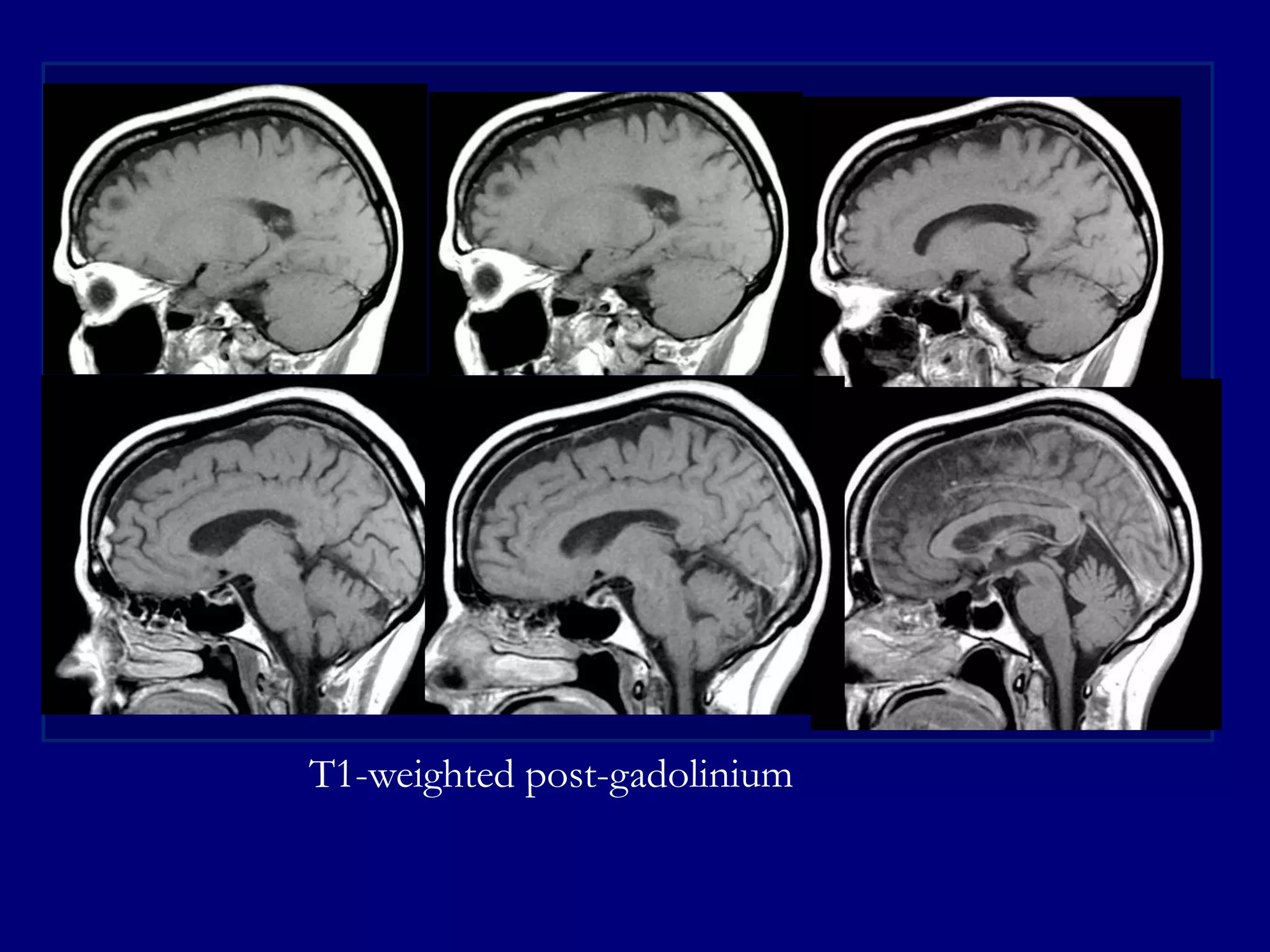
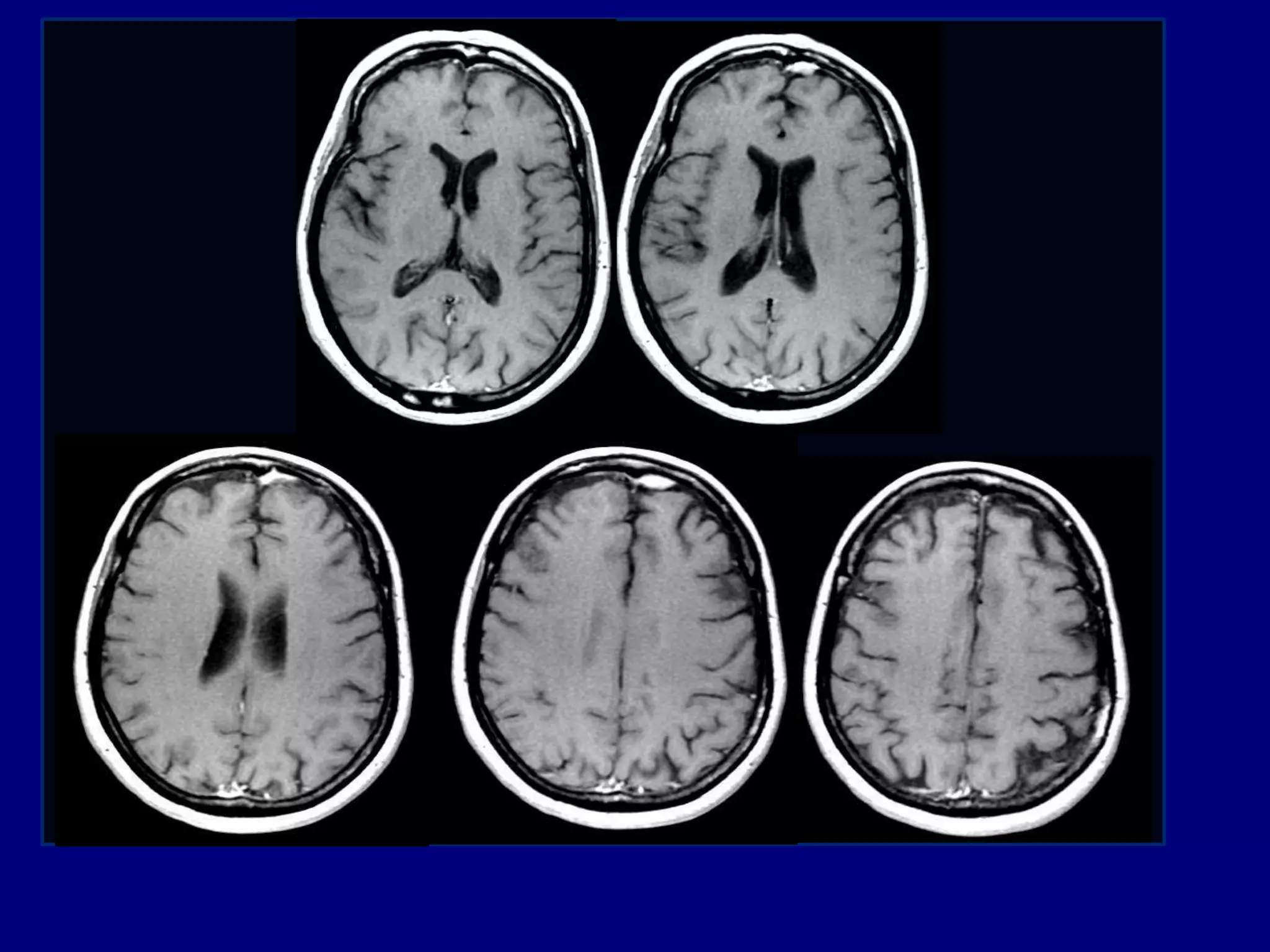
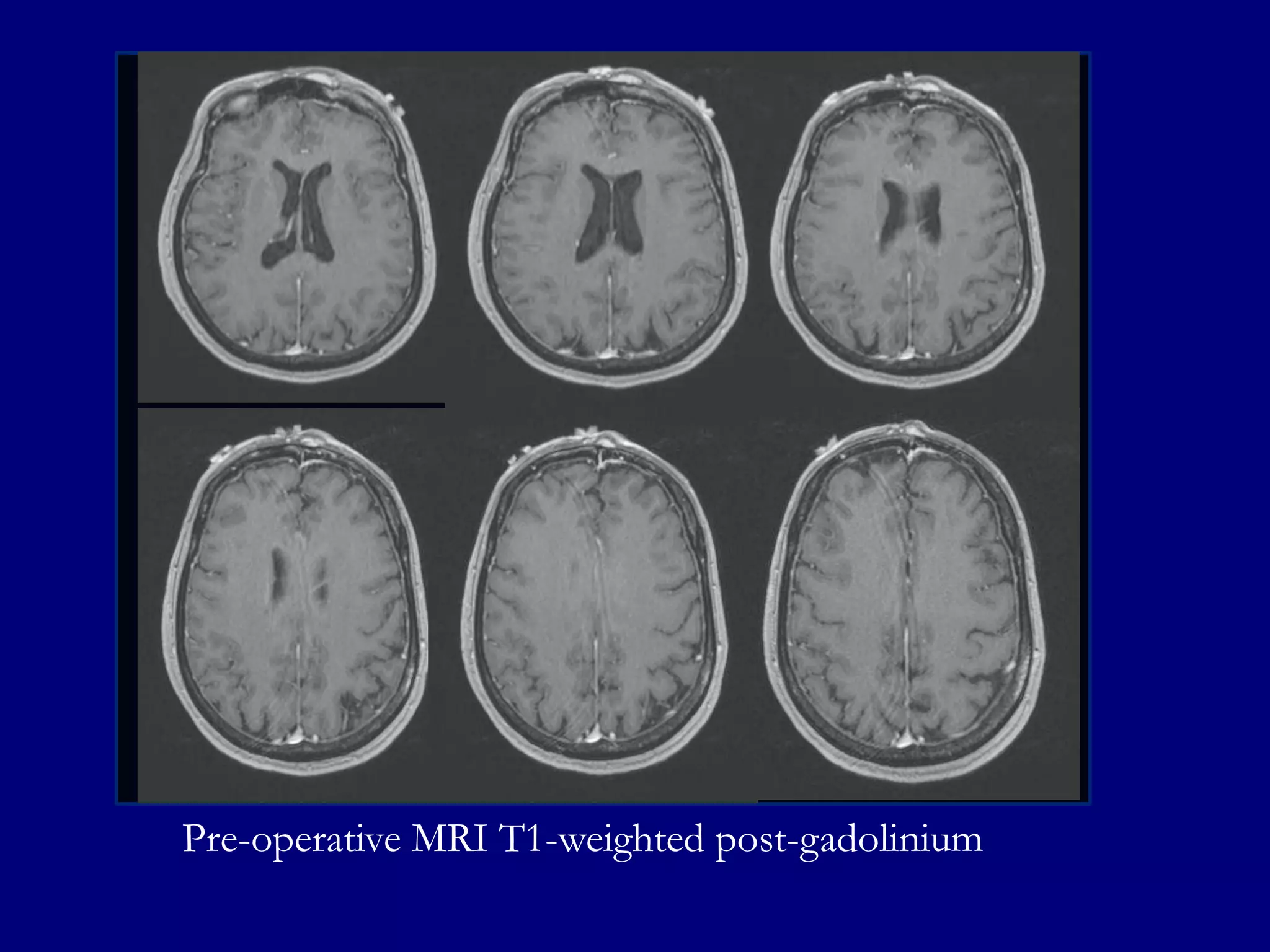
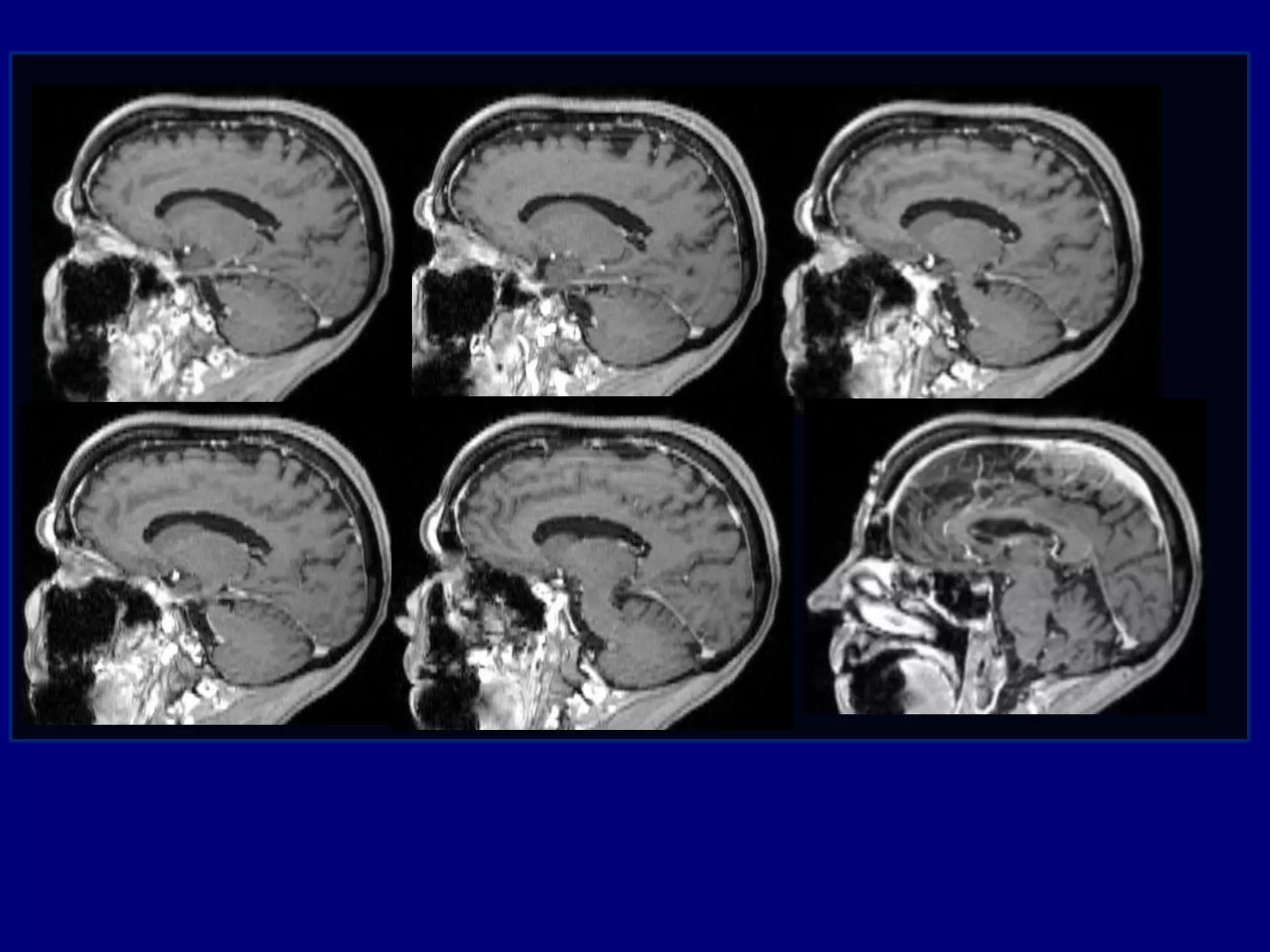
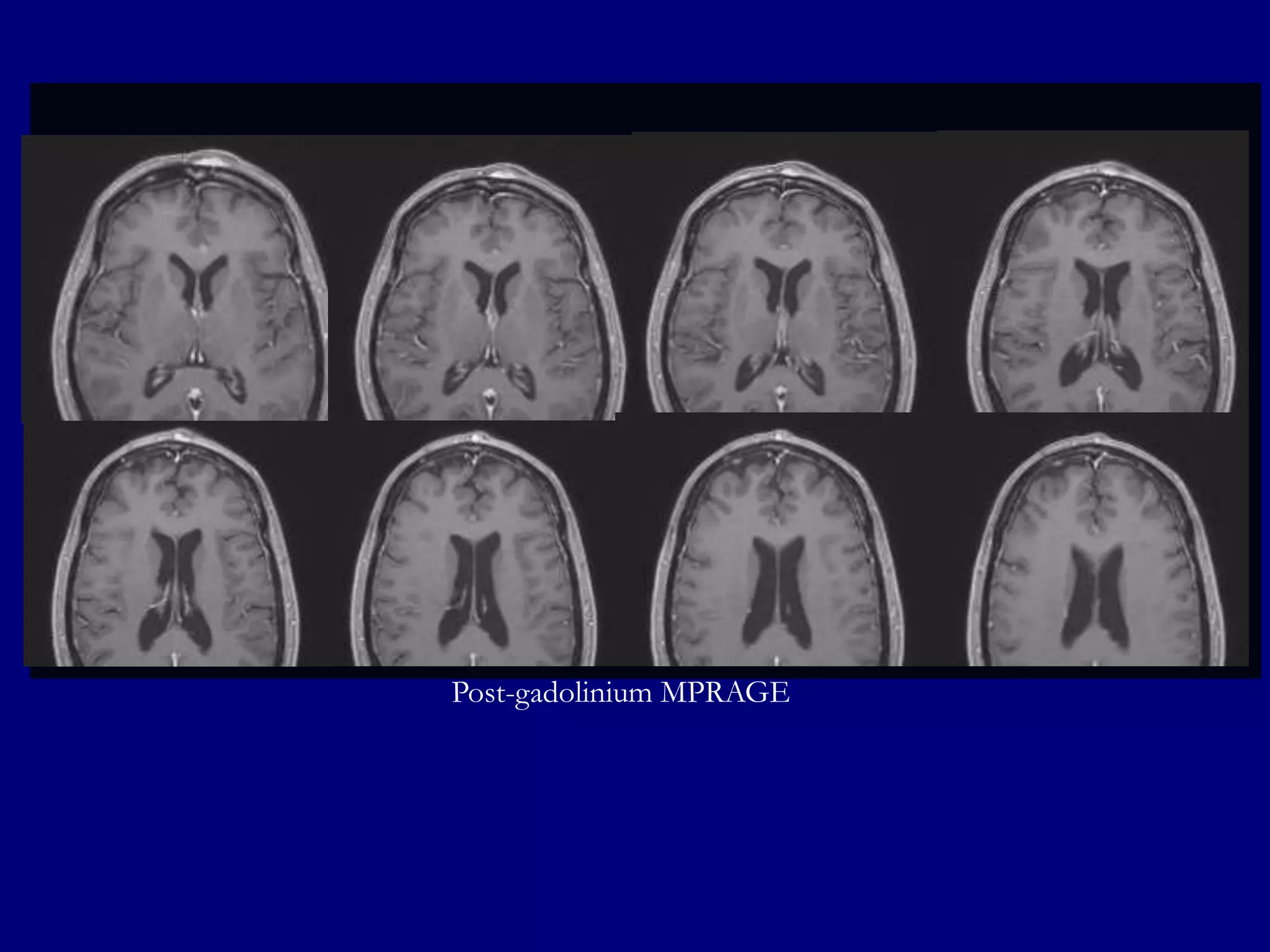
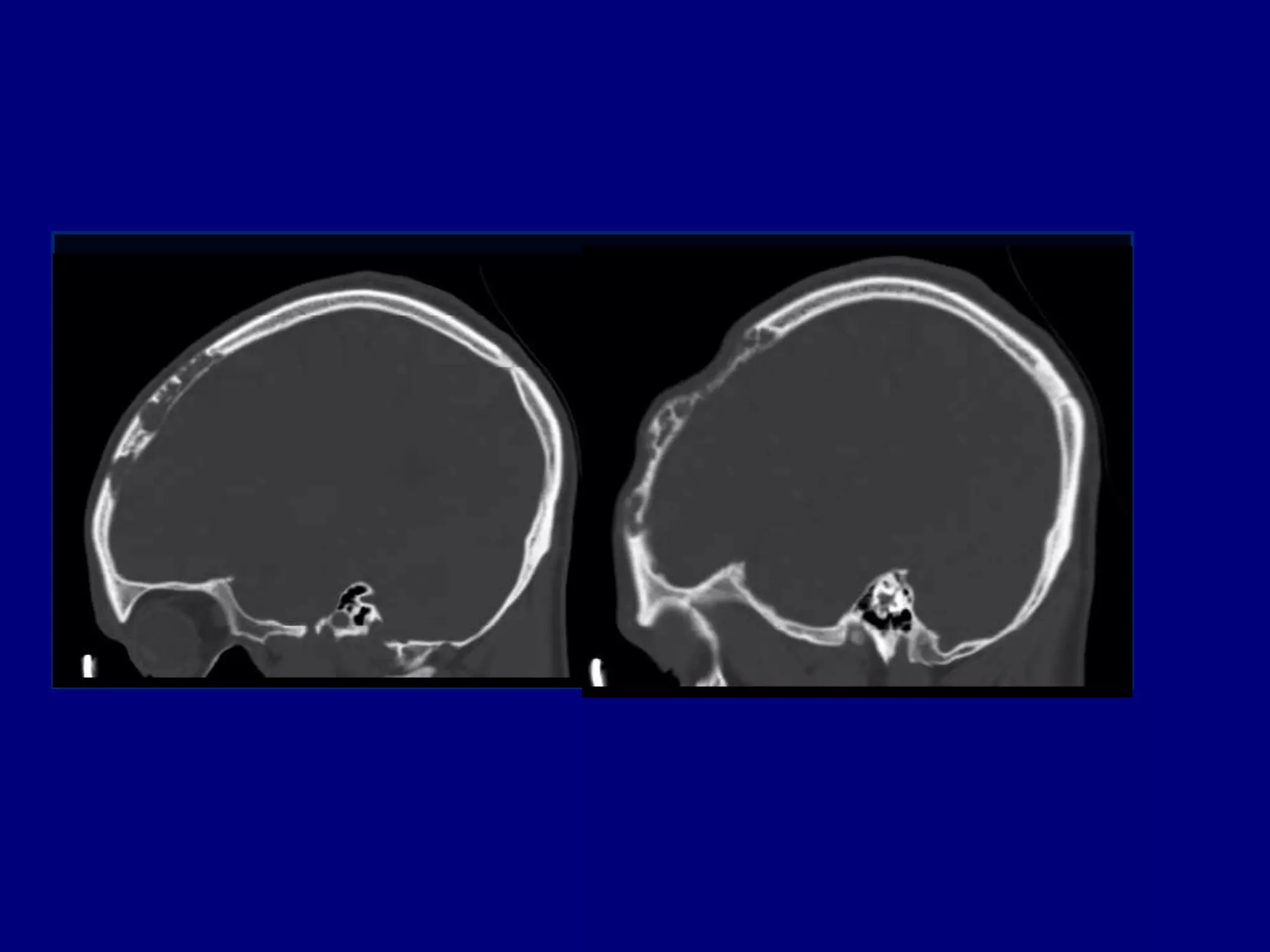
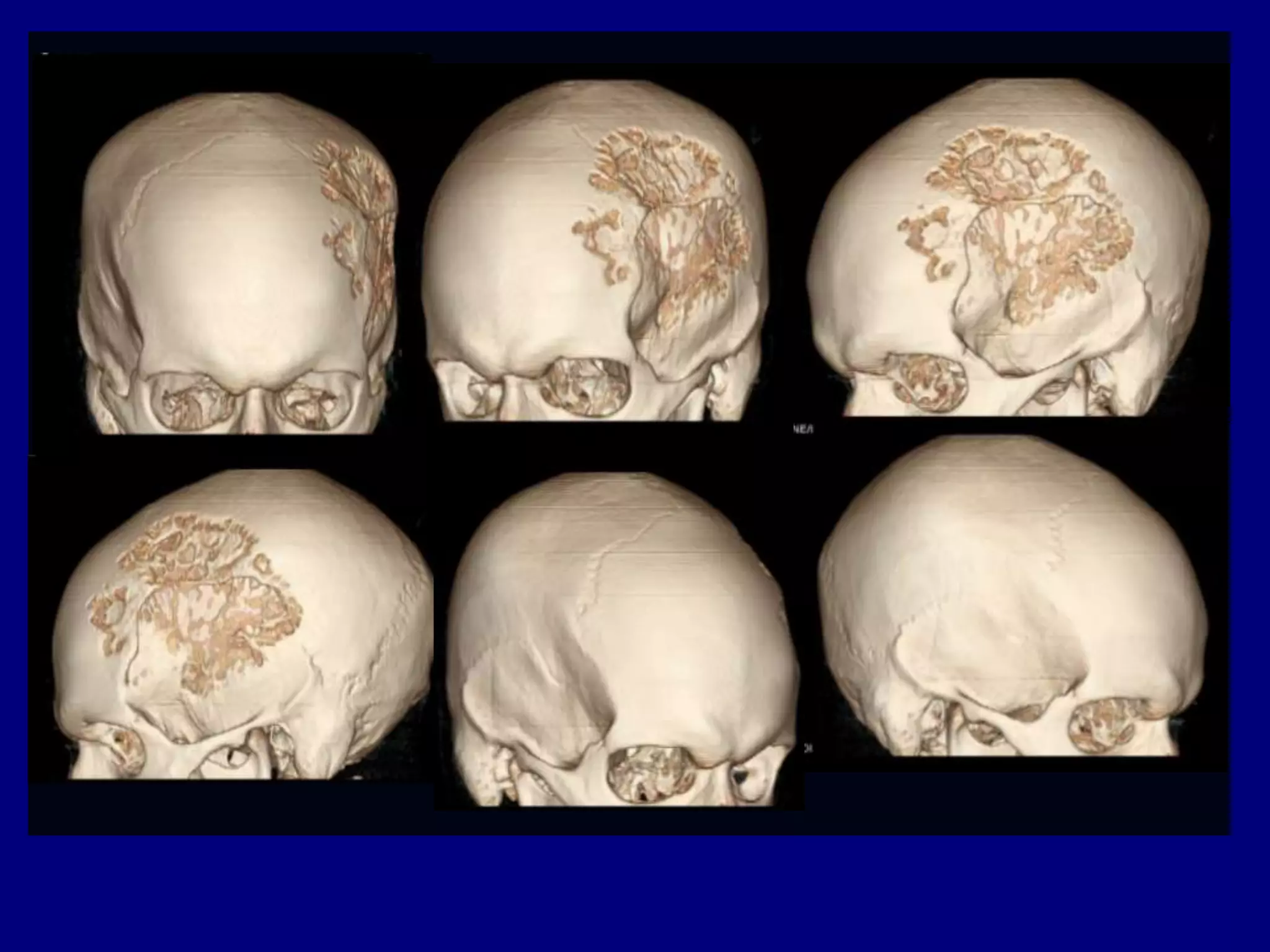
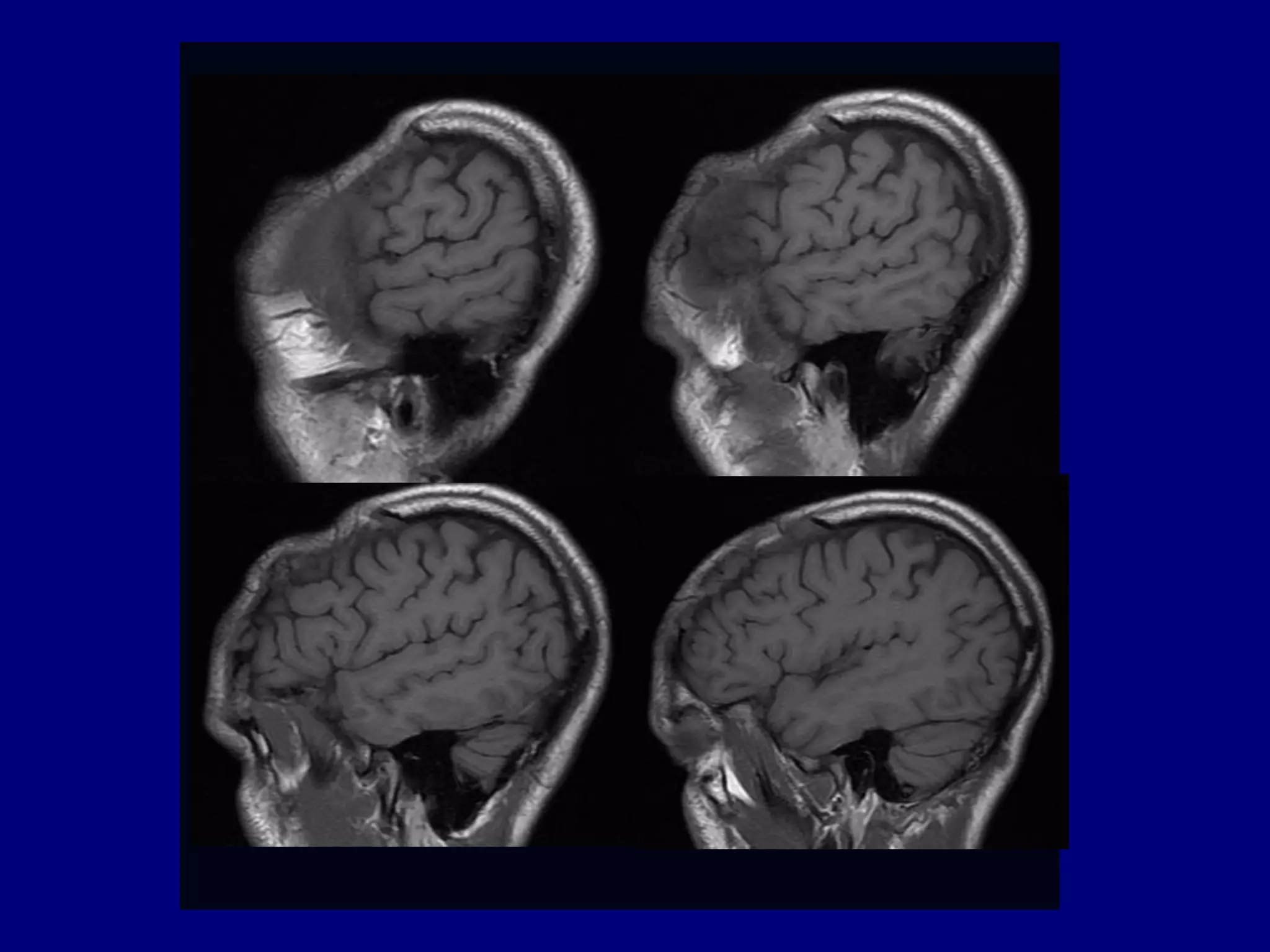
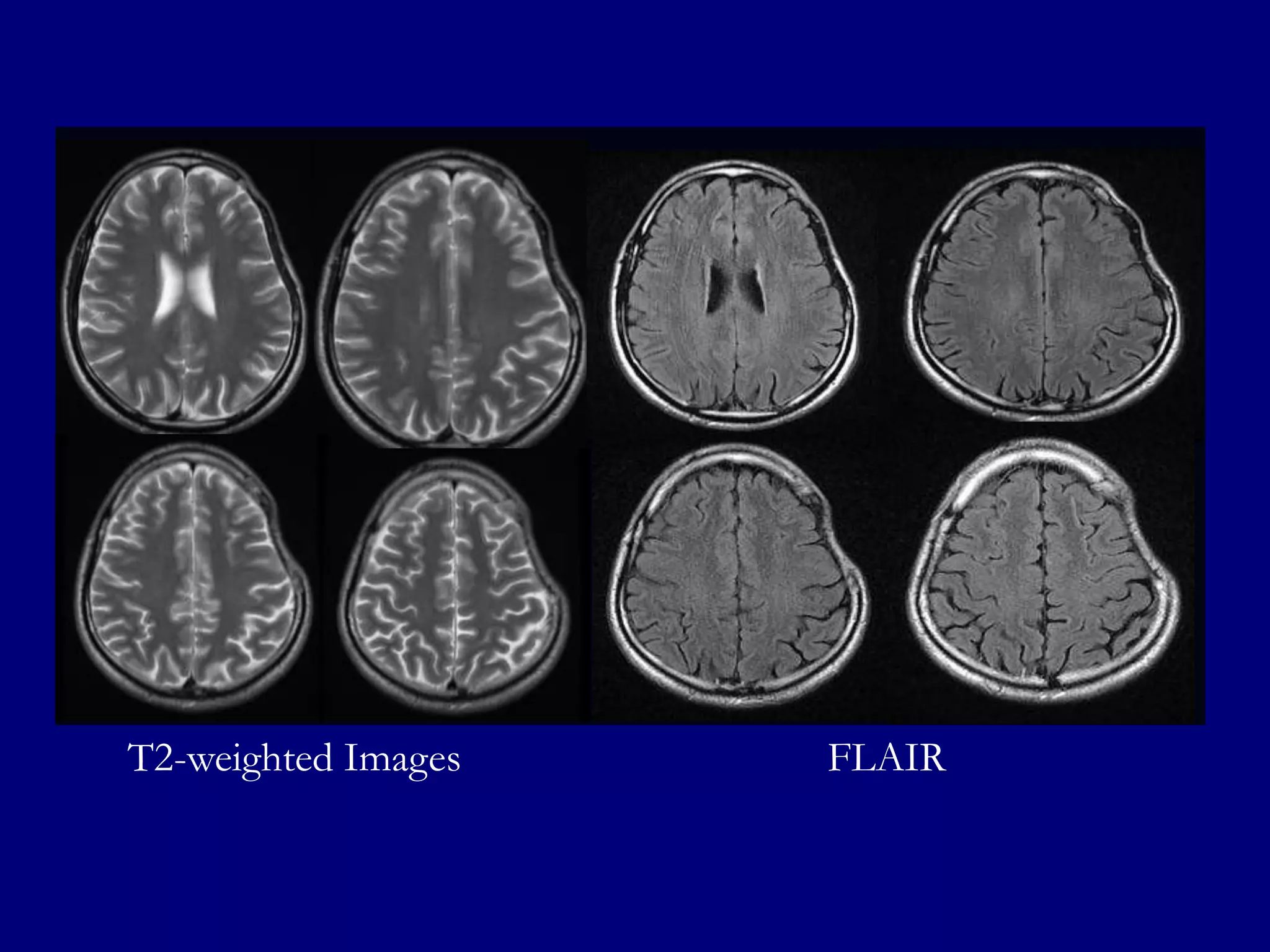
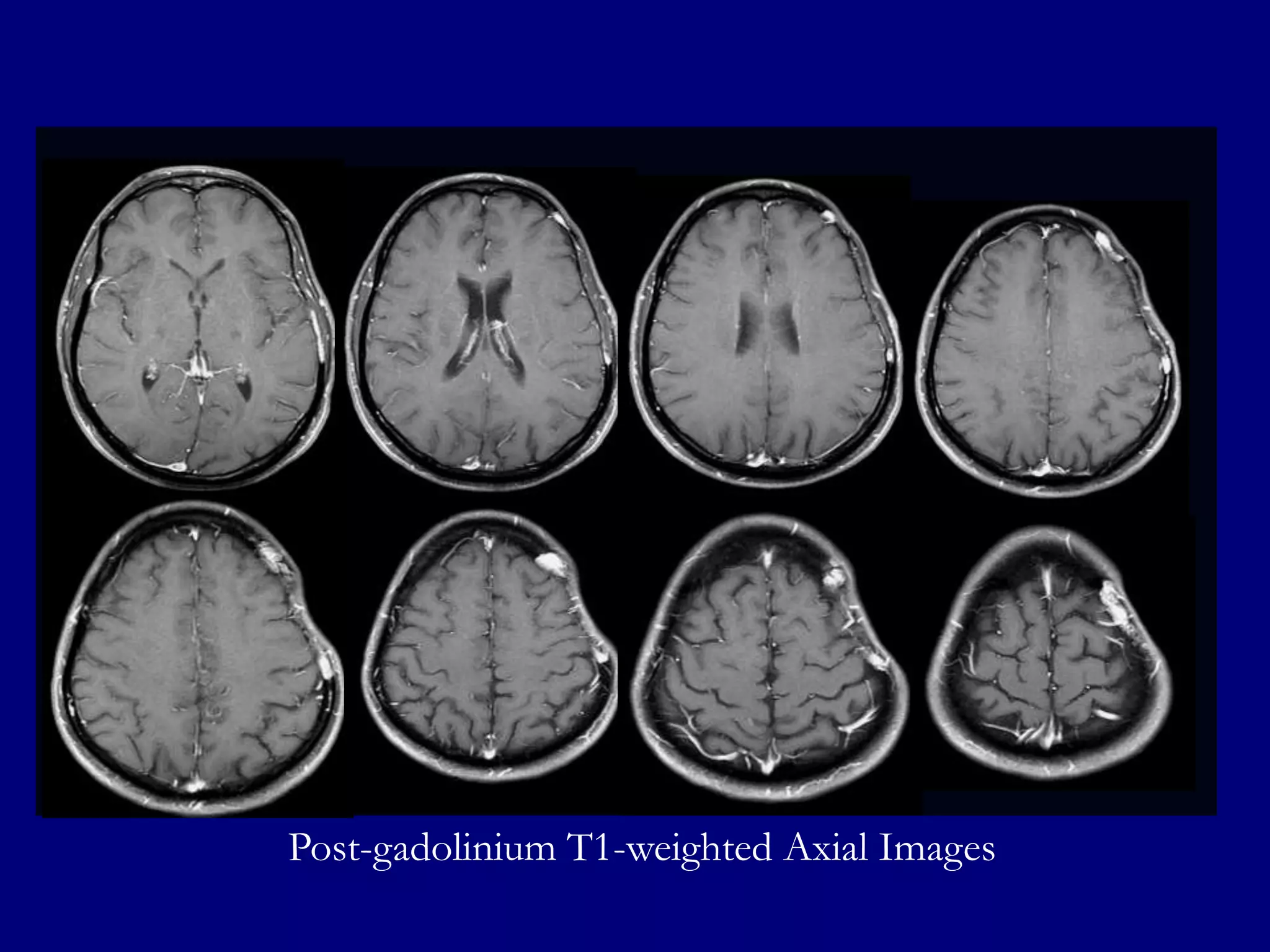
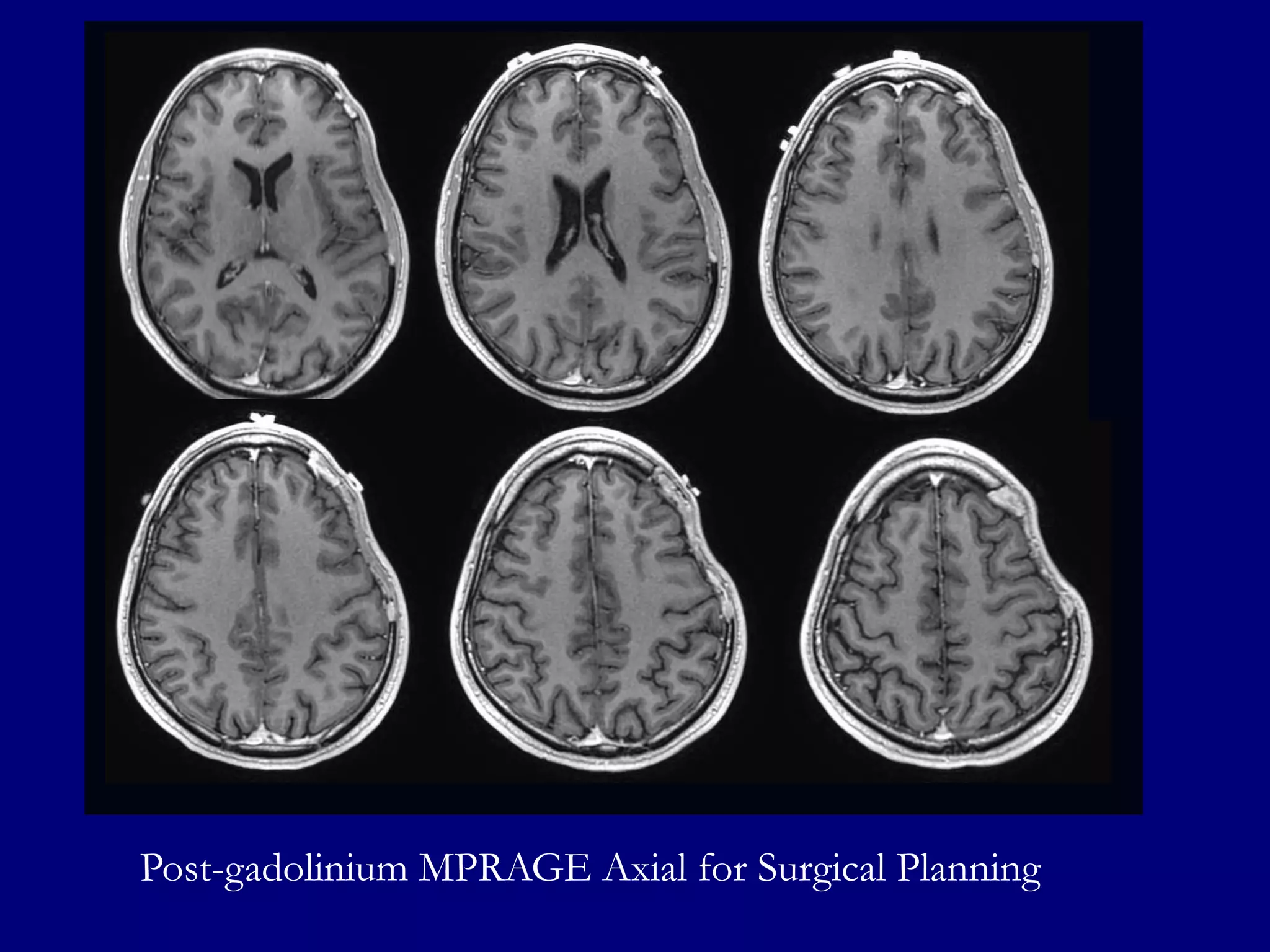
A 37-year-old man presented with right-sided numbness and headaches. Brain imaging showed hyperdense lesions in the left frontal and parietal lobes. MRI revealed well-defined hyperintense lesions on FLAIR and T2-weighted imaging that enhanced homogenously on post-gadolinium images. Spectroscopy showed an elevated choline peak. The findings were most consistent with a diagnosis of primary CNS lymphoma.