The immune system protects the body from pathogens through primary organs like the thymus and bone marrow, and secondary organs like the spleen and lymph nodes. It uses innate defenses like physical barriers and acquired defenses through active and passive immunity. When injured, the body responds through inflammation mediated by histamine, leukotrienes, prostaglandins, and platelet activating factor. HIV infects and depletes CD4+ T-cells, leading to opportunistic infections as cellular and humoral immunity declines. While there is no cure for HIV/AIDS, combination antiretroviral therapy can suppress the virus and prolong life.
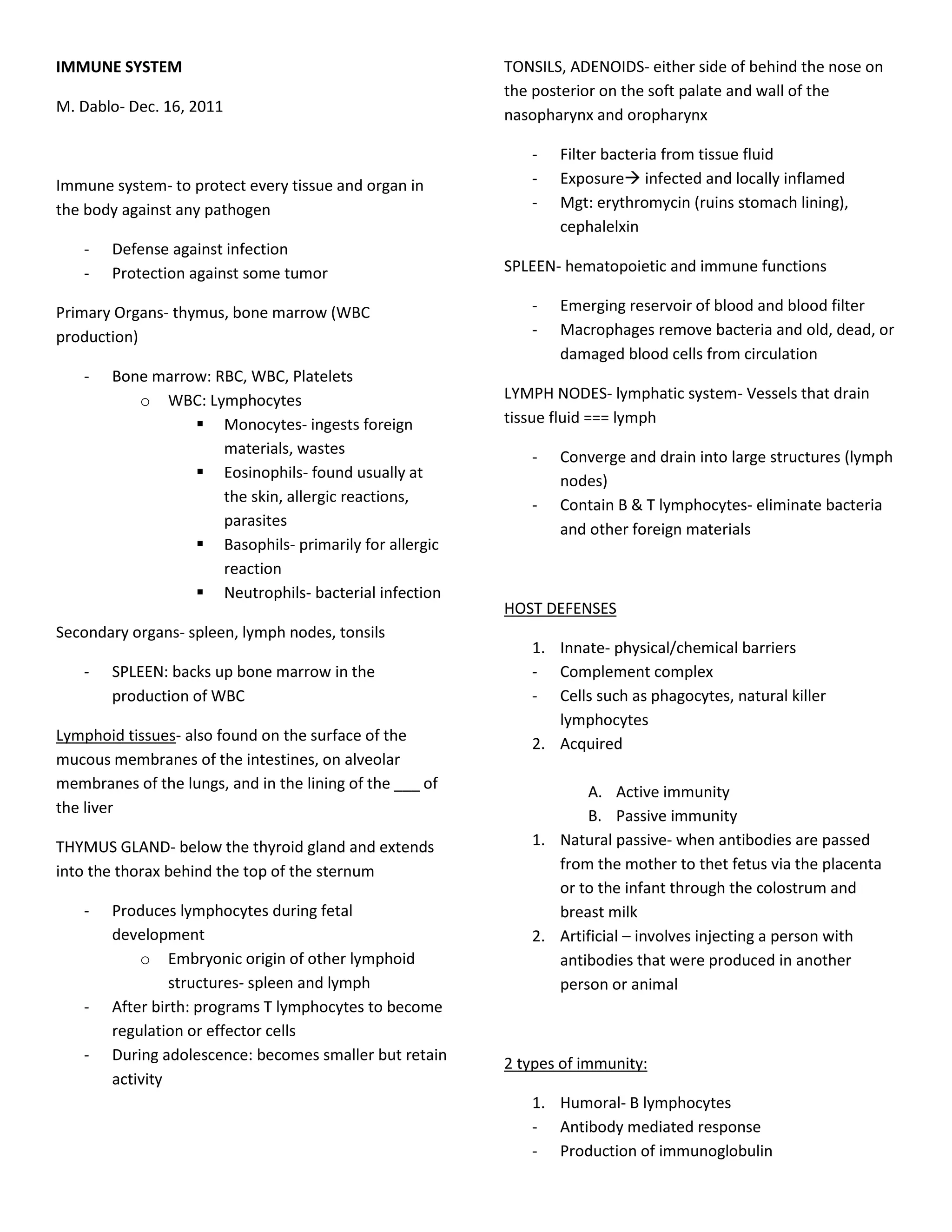

![contact with infected partner, babies from HIV - Tests conducted are confidential
+ mother
Complications:
Natural history
- Resistant HIV, repeated opportunistic
- Normal CD4 count: 800-1000/mm infections, wasting, med-related conditions,
- 2-4wwks post exposure- 50-90% with flu-like sx renal failure
[Primary HIV infxn (acute)]
AIDS Research:
- 4-6wks- seroconversion HIV +
- No cure yet due to the mutating nature of the
CxMx- peresistent cough, PCP, MTB, CMV
virus
- GI: diarrhea, wt. Loss, anorexia, enteric - Much work being done on vaccines
pathogens (salmonella, shigella) - Combination therapies- drug to boost the
- CNS: AIDS dementia/HIV encephalopathy, immune system
neuorpathies - HAART- highly active anti retroviral therapy-
- Ocular- retinopathy, blindness suppress the virus and prolong life but very
- Oral- lesions- C. Albicans, vesicles, hairy expensive
leukoplakia, oral warts –HPV, peridontitis, - Vaginal microbicides
apthous ulcers
- Malignancies: Kaposi’s sarcoma can signal the Med mgt:
final stage of HIV infxn - HAART- suppresses viral action
Dx: - Antiretroviral drugs: NRTI, NNRTI, PI, Entry
inhibitors
- History
- Blood test (>12wks) Goals of tx:
o ELISA - Improve quality of life
o Western blot- more specific - Prolong life
o Rapid HIV test - Dec viral load
o Orasure - Inc CD4 count
o Celypte HIV-1 urine EIA
o Lymphocyte panel Preventive:
o CBC
- Infections
o Presence of indicator dse
o PCP- started with CD4 <200 Dactrim
o Neuropsychological testing
o M. Avium complex- CD4 <50
o Viral load
Azithromycin, clarithromycin
HIV antibody test - Vaccinations
o TB- PPD
- Looks for antibodies in the blood, not the HIV o PCP- pneumovax
virus o Influenza- flu vaccine
- Must be accompanied by pre- and post- test
counseling Standards of care
- Window period- the period during which
- Universal precaution
antibodies cannot be detected despite the
- Protect confidentiality
possible presence of HIV, can be up to six
- Medication compliance
months but a person with HIV is infectious from
- Nonjudgmental attitude
early stage](https://image.slidesharecdn.com/immunesystem-120121235436-phpapp02/85/NCM-notes-Immune-system-3-320.jpg)
