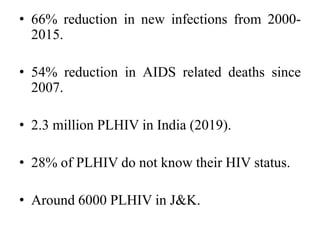
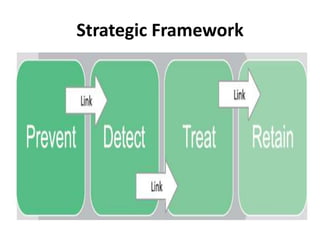
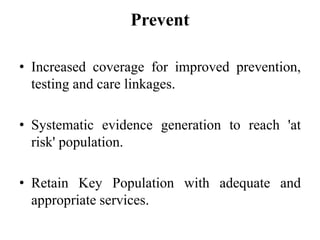
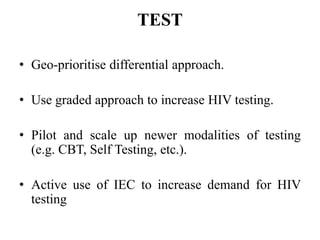
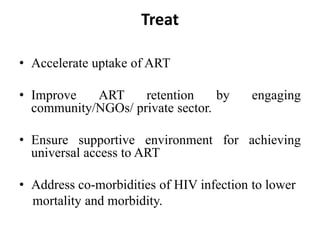
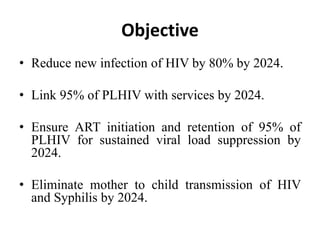
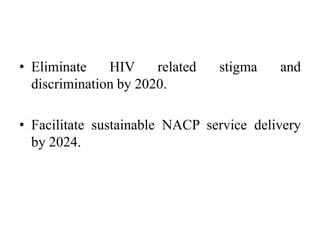
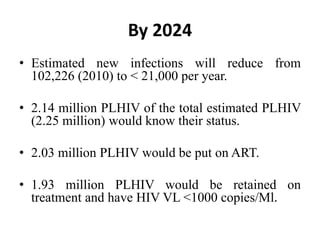
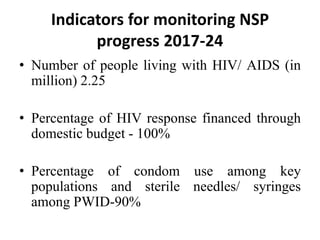
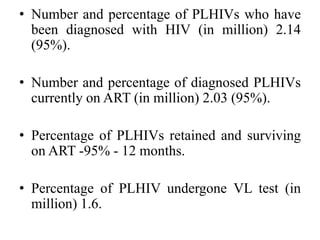
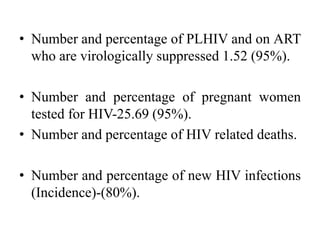
The National Strategic Plan for HIV/AIDS and STI 2017-2024 in India aims to achieve an AIDS-free India through universal access to prevention, treatment, and care services by 2024. Key goals include reducing new HIV infections by 80% and ensuring 95% of people living with HIV are aware of their status and on antiretroviral treatment. The plan leverages integration with public health systems and engages the private sector to expand testing, treatment, and prevention of mother-to-child transmission of HIV. Progress will be monitored based on indicators like the percentage of people on treatment who are virally suppressed and the reduction in new infections and HIV-related deaths.