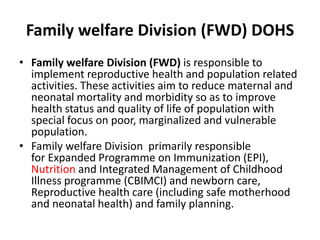
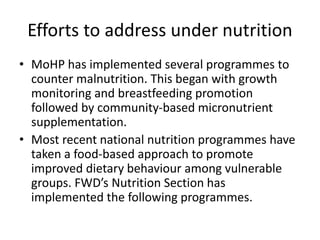
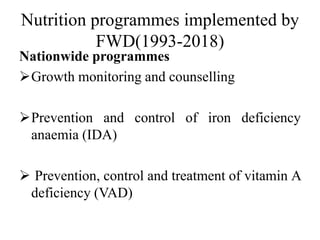
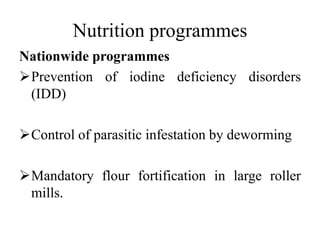
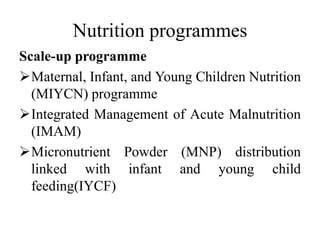
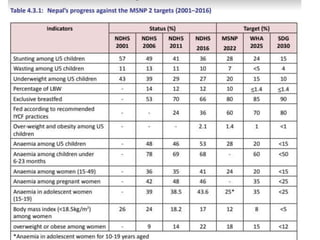
The National Nutrition Programme in Nepal aims to improve the nutritional status of its citizens, particularly focusing on vulnerable populations including children, pregnant women, and adolescents. It encompasses a variety of nutrition-related initiatives and programs to address malnutrition and promote health, aligning with global and national strategic frameworks. The program emphasizes collaborative efforts across sectors to address both under-nutrition and over-nutrition, while also targeting specific health outcomes aligned with sustainable development goals.