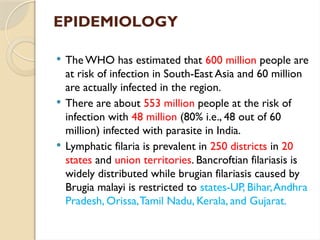
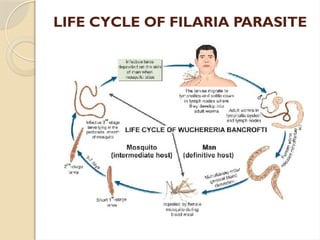
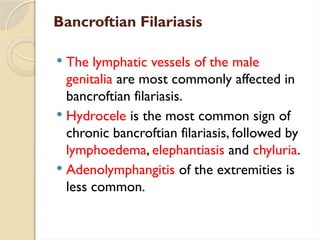
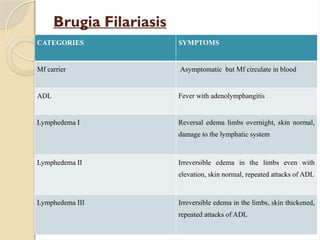
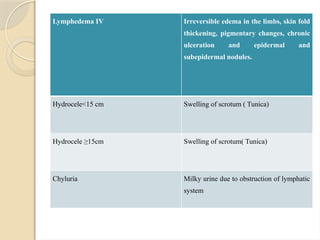
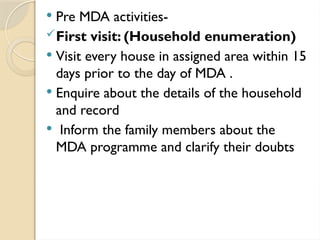
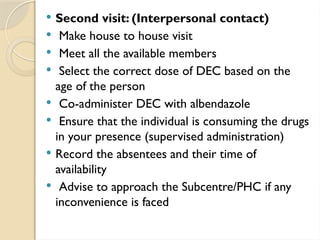
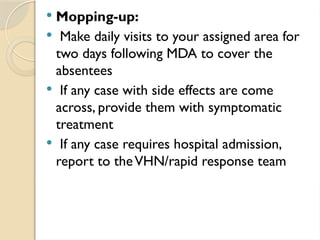
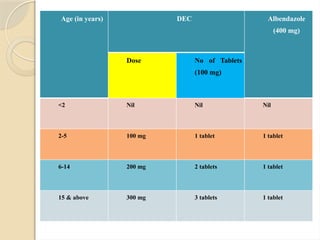
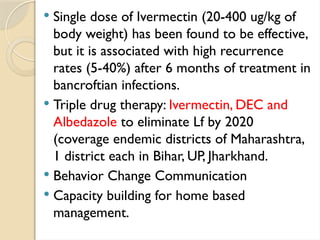
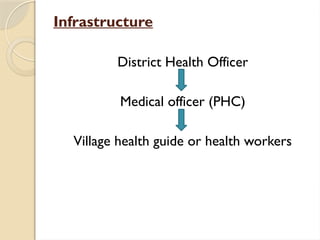
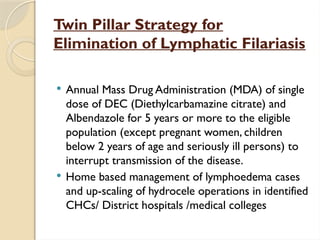
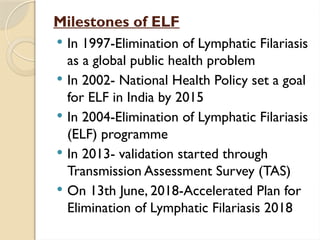
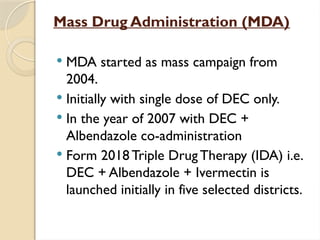
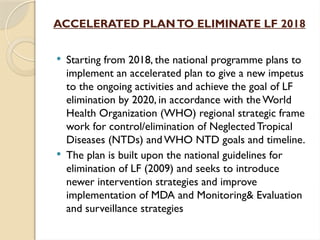
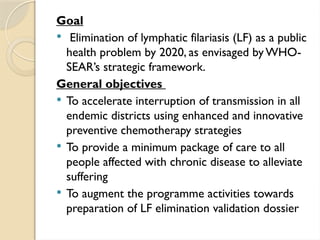
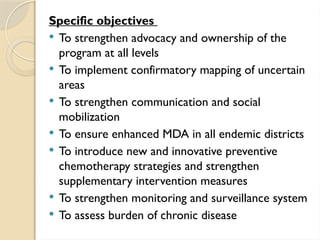
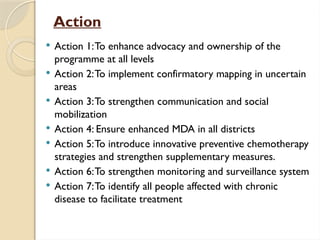
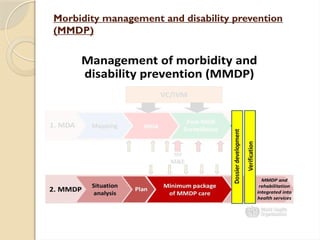
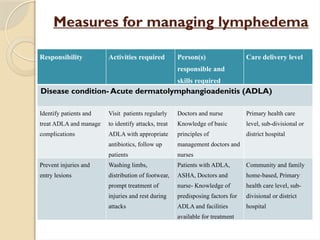
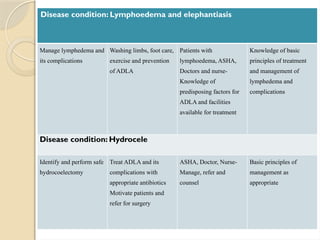
The seminar discusses the National Filaria Control Programme (NFCP) launched in India in 1955 to combat lymphatic filariasis, a disease caused by parasitic worms transmitted by mosquitoes. It highlights the disease's epidemiology, symptoms, and the strategies for control, including mass drug administration and community engagement. The goal is to eliminate lymphatic filariasis as a public health issue by 2020, supported by innovative treatment methods and a comprehensive management plan for affected individuals.