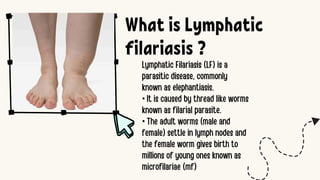
Lymphatic Filariasis
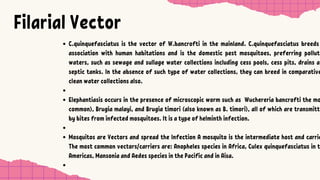
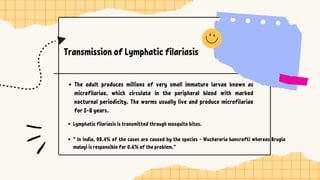
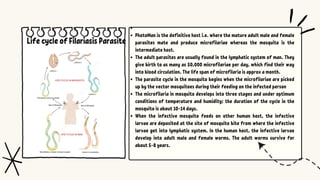
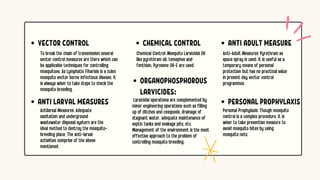
Lymphatic filariasis, commonly known as elephantiasis, is a neglected tropical disease caused by thread-like parasitic worms such as Wuchereria bancrofti, Brugia malayi, and Brugia timori. These parasites are transmitted to humans through the bite of infected mosquitoes, primarily from the Culex, Anopheles, or Aedes species.
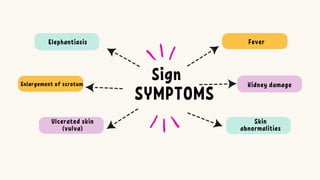
Once inside the body, the larvae migrate to the lymphatic system, where they mature into adult worms and cause blockages. This leads to swelling, usually in the legs, arms, breasts, or genitals, resulting in severe disfigurement and disability. The disease often causes pain, social stigma, and economic hardship due to its chronic nature and the loss of productivity.
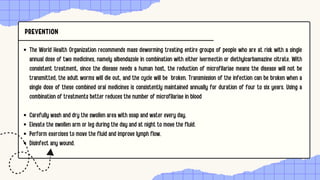
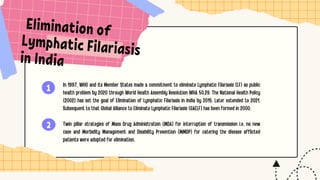
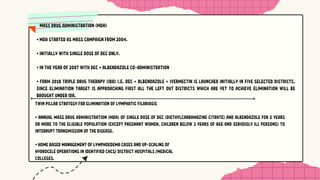
Though the infection may be asymptomatic for years, it can still cause damage to the lymphatic system and kidneys. Mass drug administration (MDA) programs are used to control and eventually eliminate the disease by reducing transmission. Proper hygiene, limb care, and in some cases surgery, are needed to manage chronic symptoms in affected individual