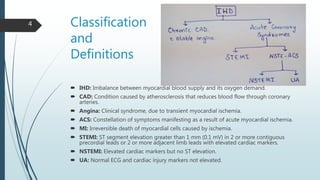
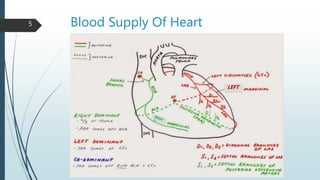
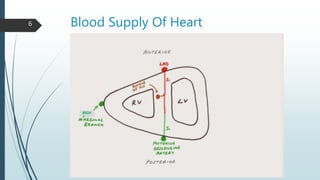
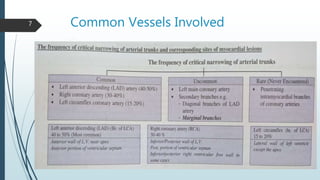
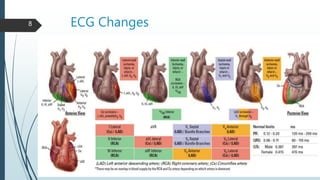
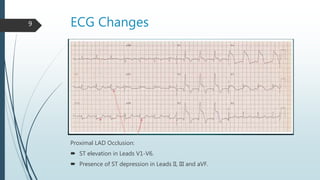
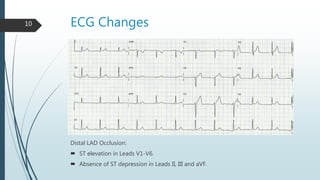
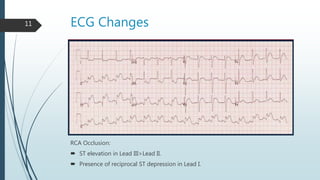
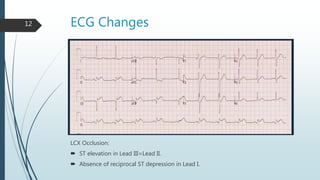
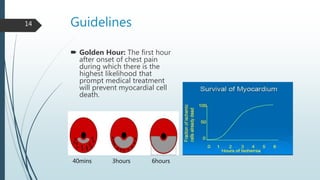
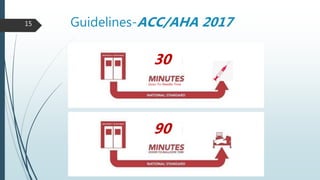
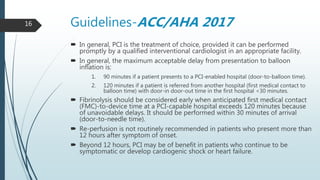
Mr. X, a 62-year-old smoker, presented to the hospital with severe chest pain. Myocardial infarction (MI), the death of heart muscle, can be classified as ST-segment elevation MI (STEMI) or non-ST-segment elevation MI (NSTEMI) based on electrocardiogram (ECG) findings. The heart receives its blood supply from the left and right coronary arteries, which are commonly blocked by blood clots. Timely reperfusion through procedures like percutaneous coronary intervention (PCI) within 90 minutes of arrival can reduce heart muscle death, as the first hour after symptoms presents the highest likelihood of preventing cell death. Guidelines recommend fibrinolysis or PCI depending on facility capabilities and