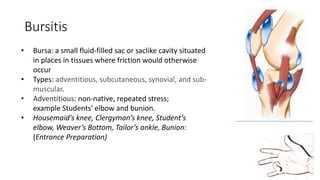
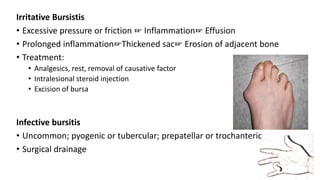
This document provides an overview of common soft tissue conditions in orthopedics, including bursitis, tendon injuries, and nerve entrapments. It discusses the anatomy, causes, symptoms, examinations, and treatment approaches for various conditions such as tennis elbow, carpal tunnel syndrome, trigger finger, and frozen shoulder. The document is intended as an educational guide for orthopedic practitioners.







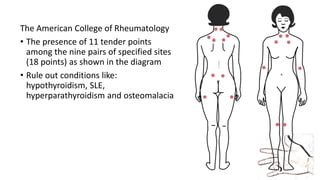
![Fibromyalgia
• Disorder of chronic, widespread pain and tenderness
• Typically presents in young or middle-aged women but can affect patients
of either sex and at any age
Signs and symptoms:
• Persistent (≥ 3 mo) widespread pain (pain/tenderness on both sides of the
body, above and below the waist, and includes the axial spine [usually the
paraspinus, scapular, and trapezius muscles])
• Stiffness
• Fatigue; disrupted and unrefreshing sleep
• Cognitive difficulties
• Multiple other unexplained symptoms, anxiety and/or depression, and
functional impairment of activities of daily living (ADLs)](https://image.slidesharecdn.com/lecturekist-151004012439-lva1-app6892/85/Lecture-kist-40-320.jpg)