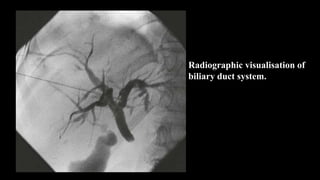
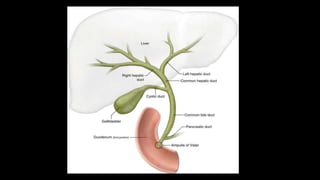
Percutaneous transhepatic cholangiography (PTC) is a radiographic procedure used to visualize the biliary duct system. It involves inserting a needle through the liver under imaging guidance and injecting contrast dye. PTC can be used diagnostically to distinguish intrahepatic and extrahepatic obstructions or therapeutically to place biliary stents. Potential complications include cholangitis, bile leaks, and hemorrhage. Proper patient preparation and post-procedure monitoring is important to reduce risks.
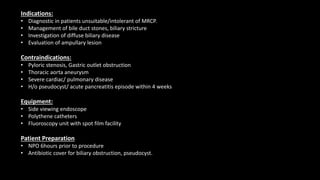
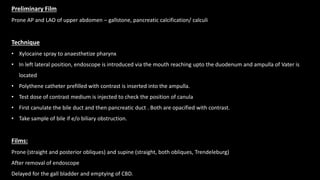
![Indications
Diagnostic:
• Prior to therapeutic intervention- biliary
drainage procedure/ stenting
• Distinguish intrahepatic cholestasis and
extrahepatic obstruction ( calculi, stricture,
malignancy).
• Biliary diseases.
Therapeutic:
• Place a percutaneous biliary stent
• Drain infected bile
Contraindications
• Bleeding diathesis :
Platelet count < 1,00,000 /mm3 and
Prothrombin time <60% of control value.
• Biliary sepsis [need of appropriate
antibiotic cover, small volume contrast,
establish drainage]
• Contrast hypersensitivity
• Severe cardiovascular and respiratory
compromise
• Severe jaundice, ascites anemia and poor
general condition of the patient.](https://image.slidesharecdn.com/bsc-221116180603-fc24fd69/85/bsc-pptx-4-320.jpg)