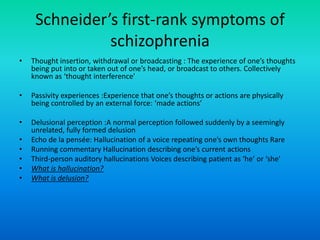
Schizophrenia is a chronic mental disorder characterized by positive and negative symptoms. It was first identified in the 1890s and has genetic and environmental risk factors. Key aspects include diagnostic criteria, types of schizophrenia, implicated neurochemicals and neural pathways, pharmacological treatments including antipsychotics, and importance of psychosocial interventions and early intervention. Non-pharmacological management includes family therapy, CBT, and vocational rehabilitation.