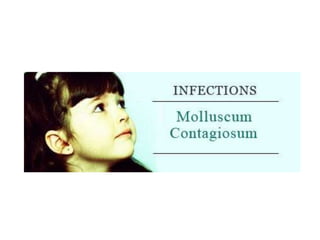
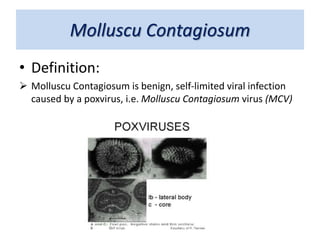
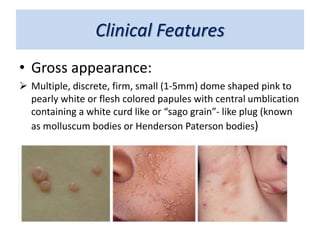
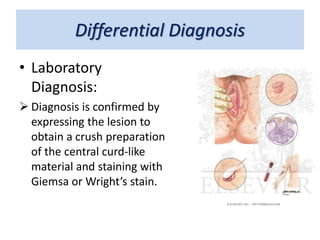
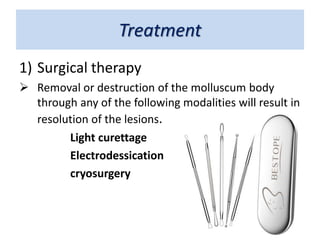
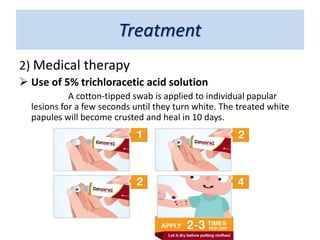
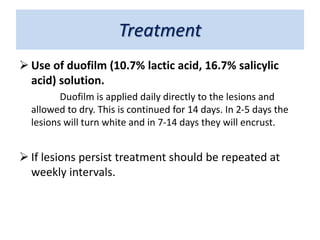
This document discusses molluscum contagiosum, a common viral skin infection caused by the molluscum contagiosum virus. It primarily affects children and sexually active adults. The infection causes multiple pink or white dome-shaped papules with a central umbilication containing a white plug. Lesions are usually found on the trunk, face, extremities and intertriginous areas in children, and the peri-anal and genital areas in adults. While self-limiting, treatment options include surgical removal or destruction of lesions through curettage, electrodessication or cryosurgery, or applying medical treatments like trichloracetic acid or lactic/salicylic acid solutions.