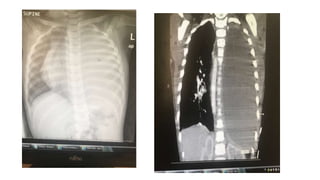
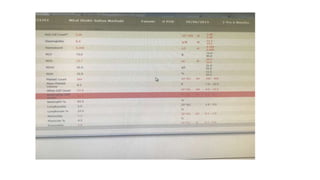
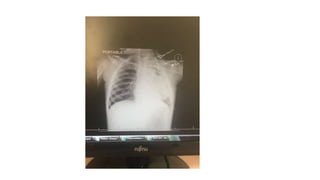
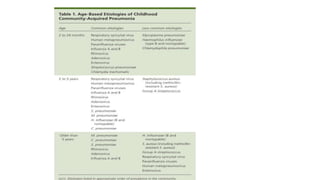
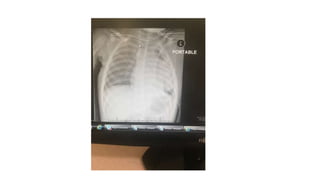
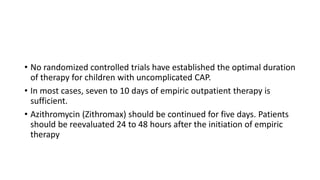
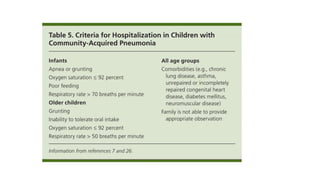
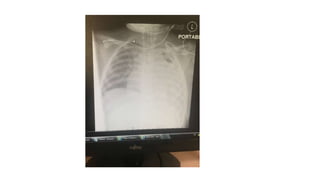
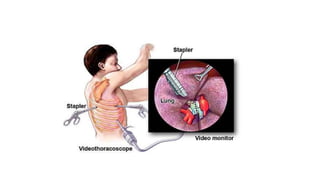
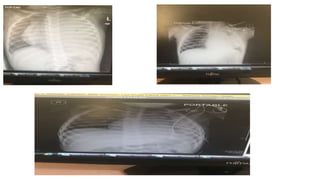
Miral is a 2.5 year old girl who has had intermittent fever and respiratory symptoms for 1 month. She has lost 1.2 kg and has decreased activity levels. Examinations suggest she has a pleural effusion that was drained, revealing 1000ml of pus. She underwent VATS surgery and is being treated with vancomycin, albumin, dexamethasone, and intubation. VATS procedures can be used to drain effusions, perform biopsies, and remove parts of the lung or tumors. Preschool aged children with pneumonia are usually treated with amoxicillin, while older children receive macrolides.