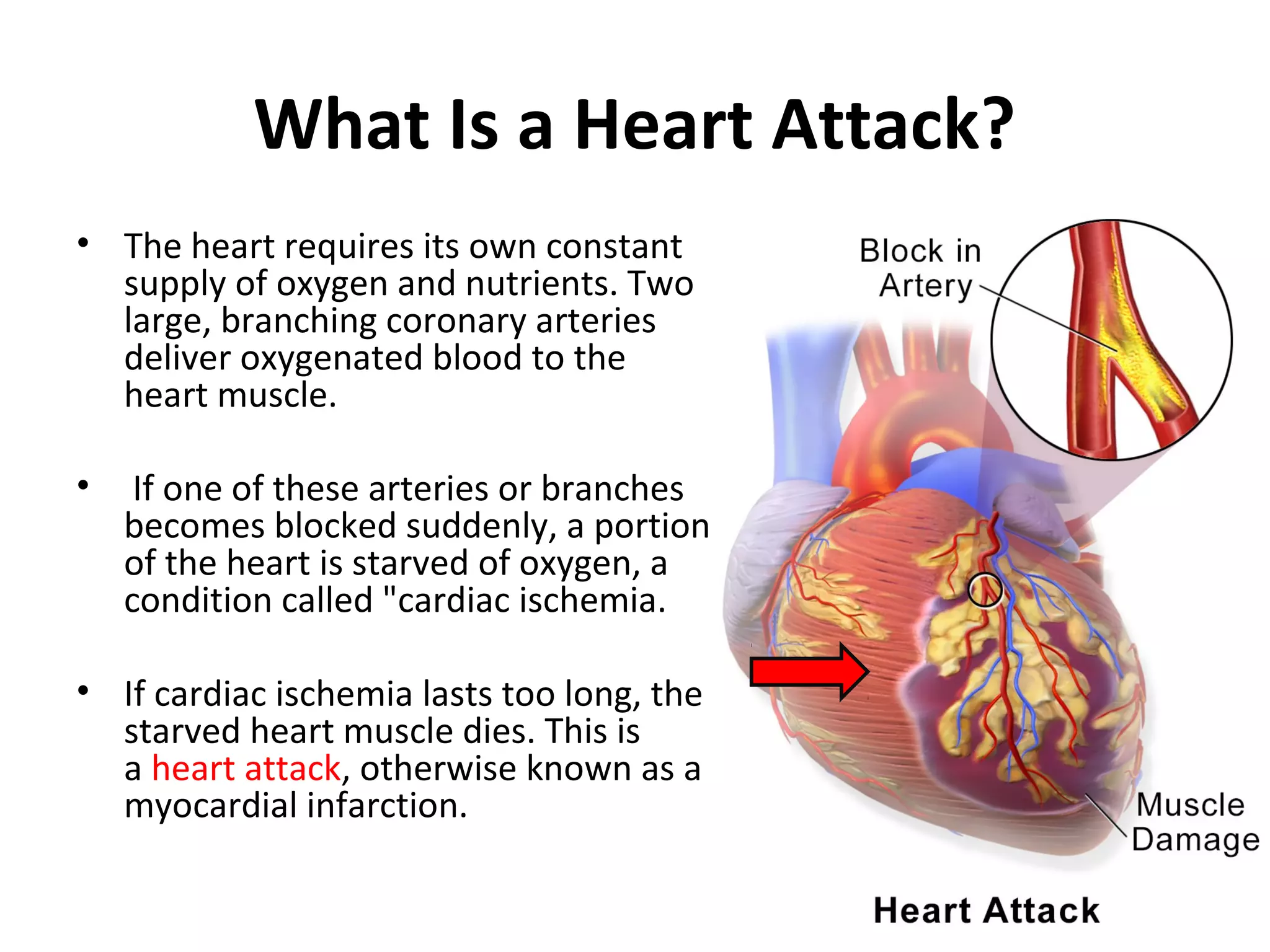
This document provides information about acute myocardial infarction (AMI) or heart attack. It defines AMI as a condition where a portion of the heart muscle dies due to lack of oxygen from a blocked artery. It describes the signs and symptoms of AMI such as chest pain and changes in vital signs. It also lists common risk factors for AMI like age, smoking, high cholesterol, and diabetes. The diagnosis involves laboratory tests, electrocardiography, and imaging of the coronary arteries. Emergency treatment focuses on oxygen, pain management, and drugs to reduce workload on the heart. Nurses monitor symptoms and vital signs, educate patients, administer medications, and ensure crash carts are prepared.