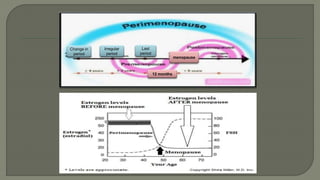
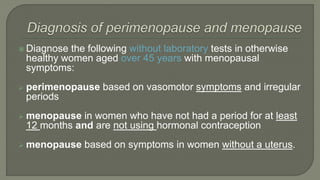
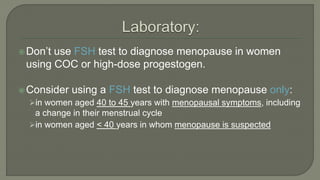
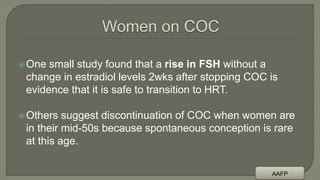
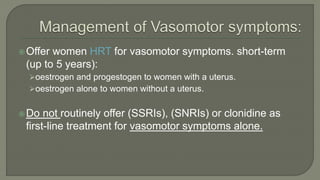
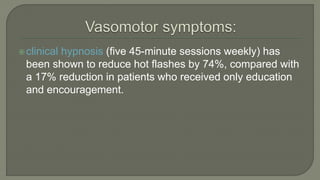
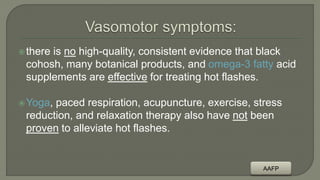
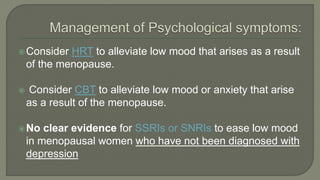
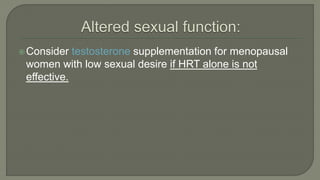
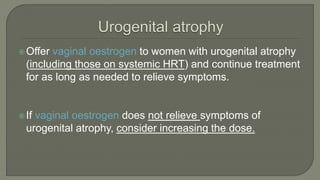
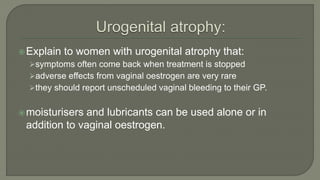
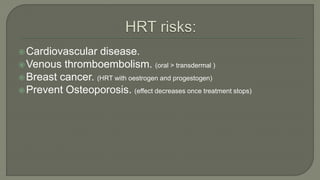
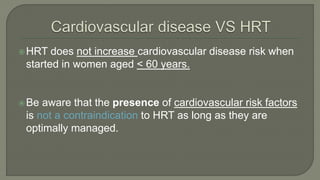
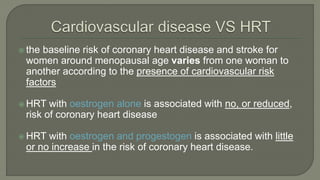
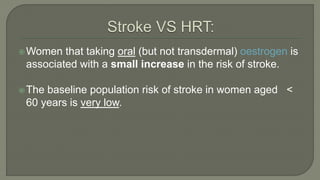
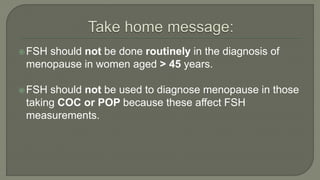
This document discusses a 52-year-old woman presenting with hot flashes and depression for 14 months without a period. It defines perimenopause, menopause and postmenopause, and lists common menopausal symptoms. It provides guidance on diagnosing and managing menopause, as well as addressing potential risks and benefits of hormone replacement therapy. Laboratory tests are not necessary to diagnose menopause in most women over age 45. Lifestyle changes and short-term hormone therapy are recommended for managing vasomotor symptoms.