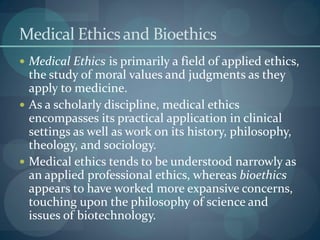
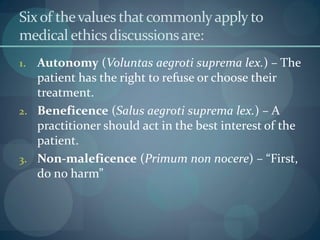
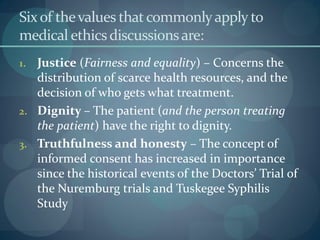
This document discusses key values and concepts in medical ethics, including autonomy, beneficence, non-maleficence, informed consent, and justice. It provides historical context on the development of medical ethics as a field. It notes that while values like autonomy, beneficence and non-maleficence provide a framework, they do not always give clear answers when they conflict in a particular situation, creating ethical dilemmas.