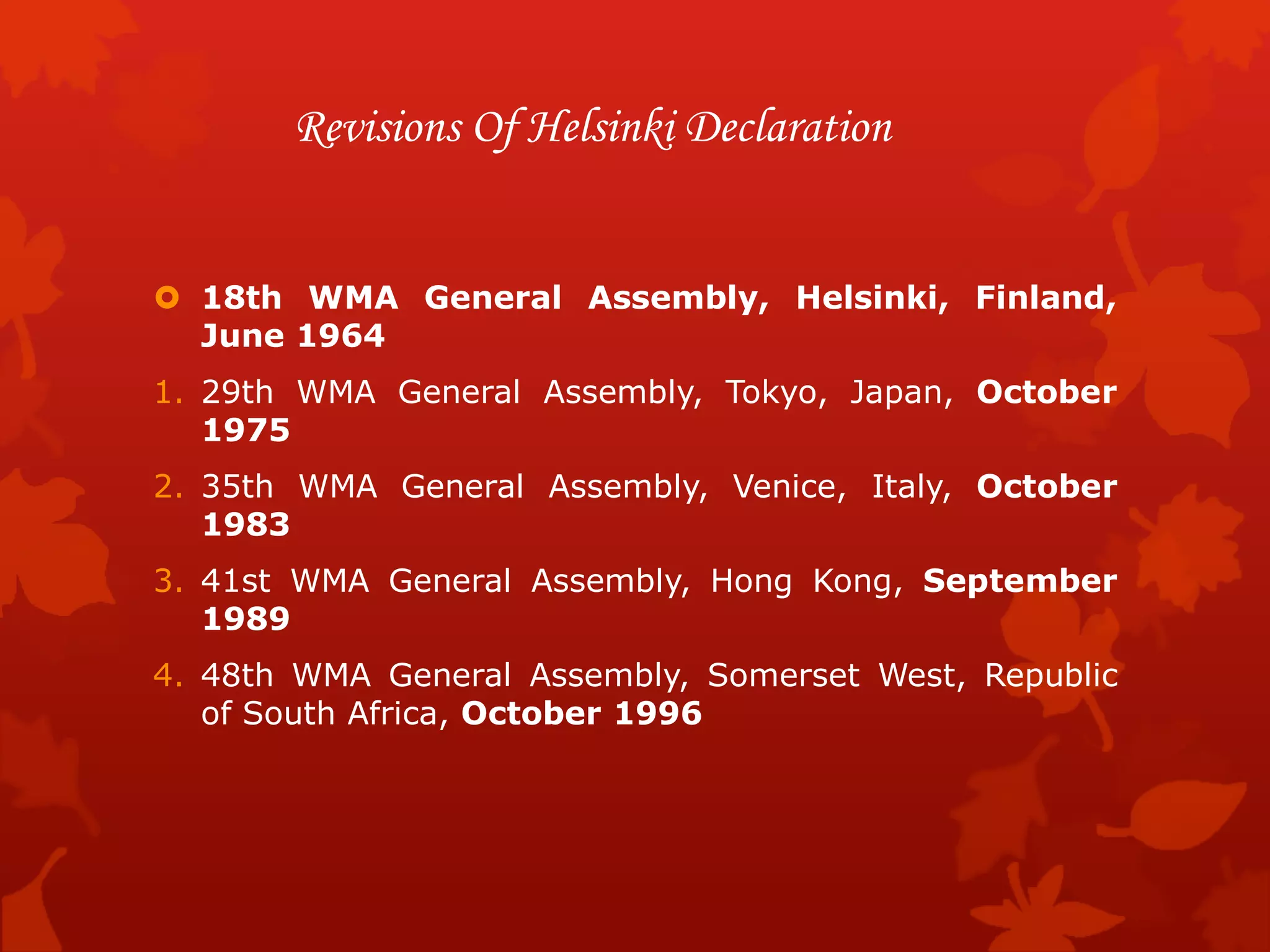
The Declaration of Helsinki is a set of ethical principles regarding human experimentation set forth by the World Medical Association. It was originally adopted in 1964 and aims to provide guidance to physicians and researchers. The Declaration establishes standards to ensure medical research involving human subjects respects their life, health, dignity, integrity, and rights. It requires voluntary informed consent and oversight by research ethics committees. The Declaration has undergone several revisions to update and clarify its guidelines as medical research has advanced. It continues to be recognized as a fundamental document for ethics in human subject research.