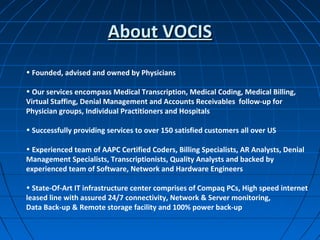
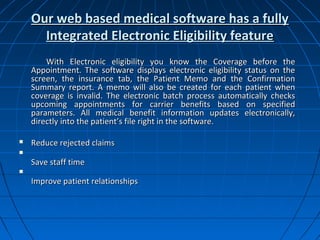
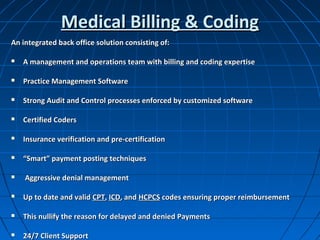
Vocis provides comprehensive medical billing, coding, and collections services for healthcare offices, focusing on cost savings and improved operational efficiency. Their offerings include medical transcription, denial management, and a web-based software solution that enhances patient experience and reduces claim rejections. Backed by a certified team and state-of-the-art IT infrastructure, Vocis supports over 150 clients across the U.S.