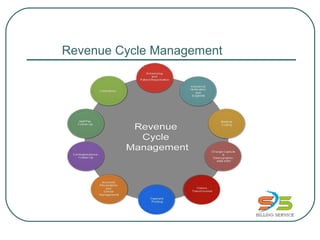
This document provides an overview of a company's revenue cycle management services. It discusses their experienced team, the full scope of services they provide including medical billing, coding, insurance verification and collections. It outlines their unique process for outsourcing these services which includes analyzing needs, establishing pilot programs, and specialized oversight teams. Graphical representations are also included showing the overall billing cycle and common reports generated from their services. Their specialties in various medical fields are listed at the end.














![AR/Denial
We clearly understand account receivable is the vital part of any business. Our experienced
billers use various follow-up methodologies to ensure prompt payment.
We run aging reports to categorize [Oldest to Latest & Highest to Lowest] outstanding claims
and follow-up with carriers. We help improve revenue realization.
Denial Management
We conduct thorough analysis of every denied claim, make the necessary corrections, and
follow-up to convert it into a clean claim.
We help improved revenue realization.
We help introduce preventive measures for future billing.
We keep a good track of outstanding accounts and follow-up on time providing maximized
revenues.
We have established clear productivity and performance metrics helping our clients to have
total control of the process and results.](https://image.slidesharecdn.com/revenuecyclemanagement-updated-180607233214/85/Revenue-cycle-management-updated-16-320.jpg)



