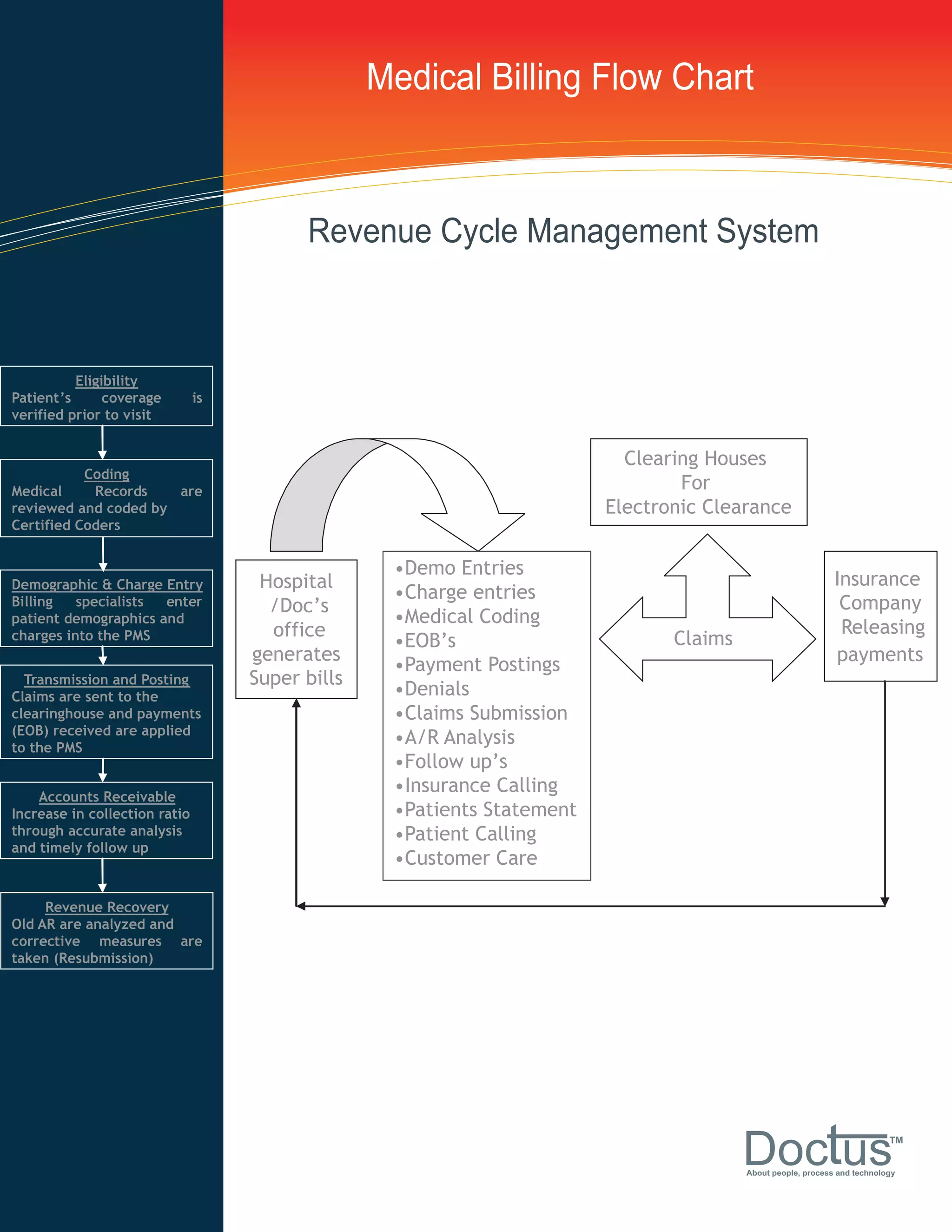
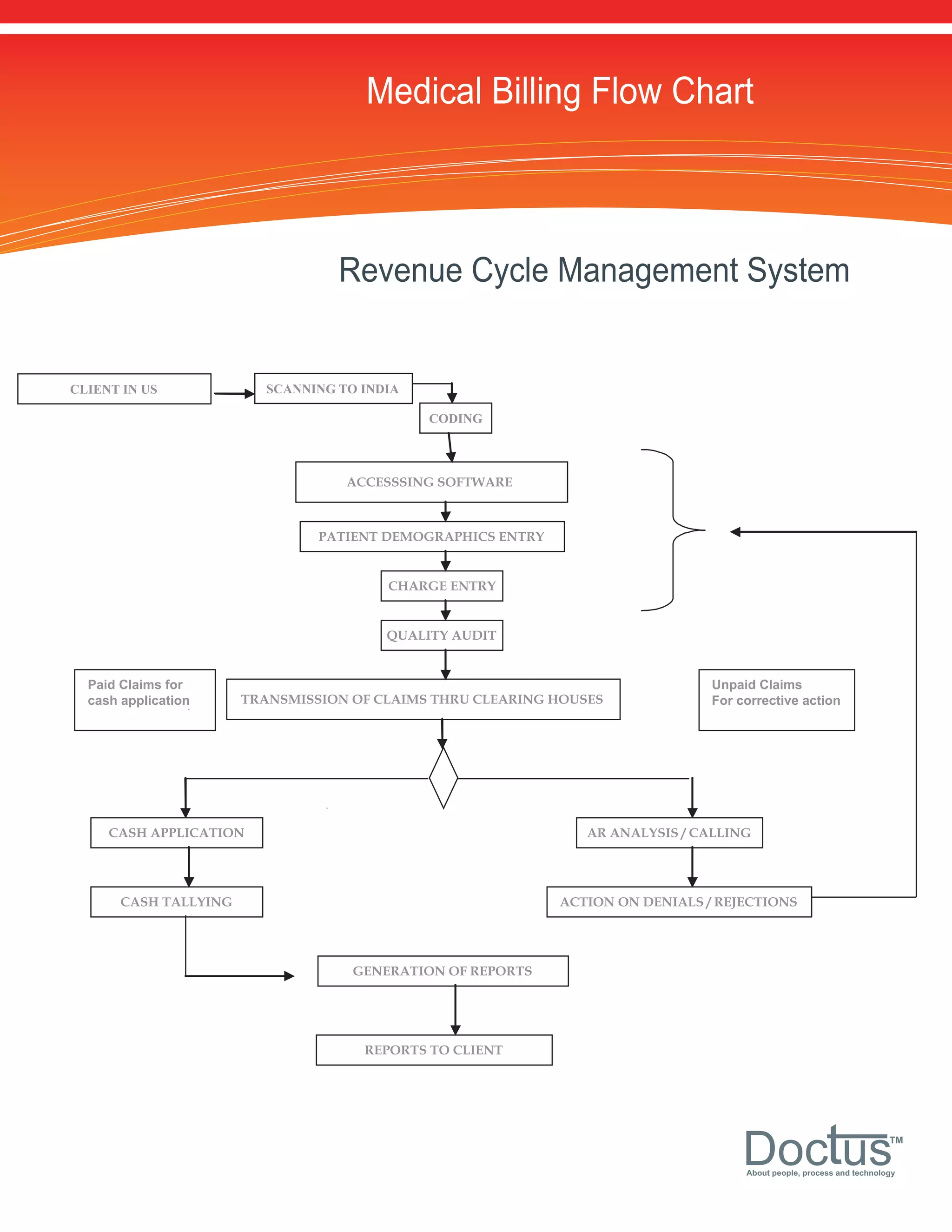
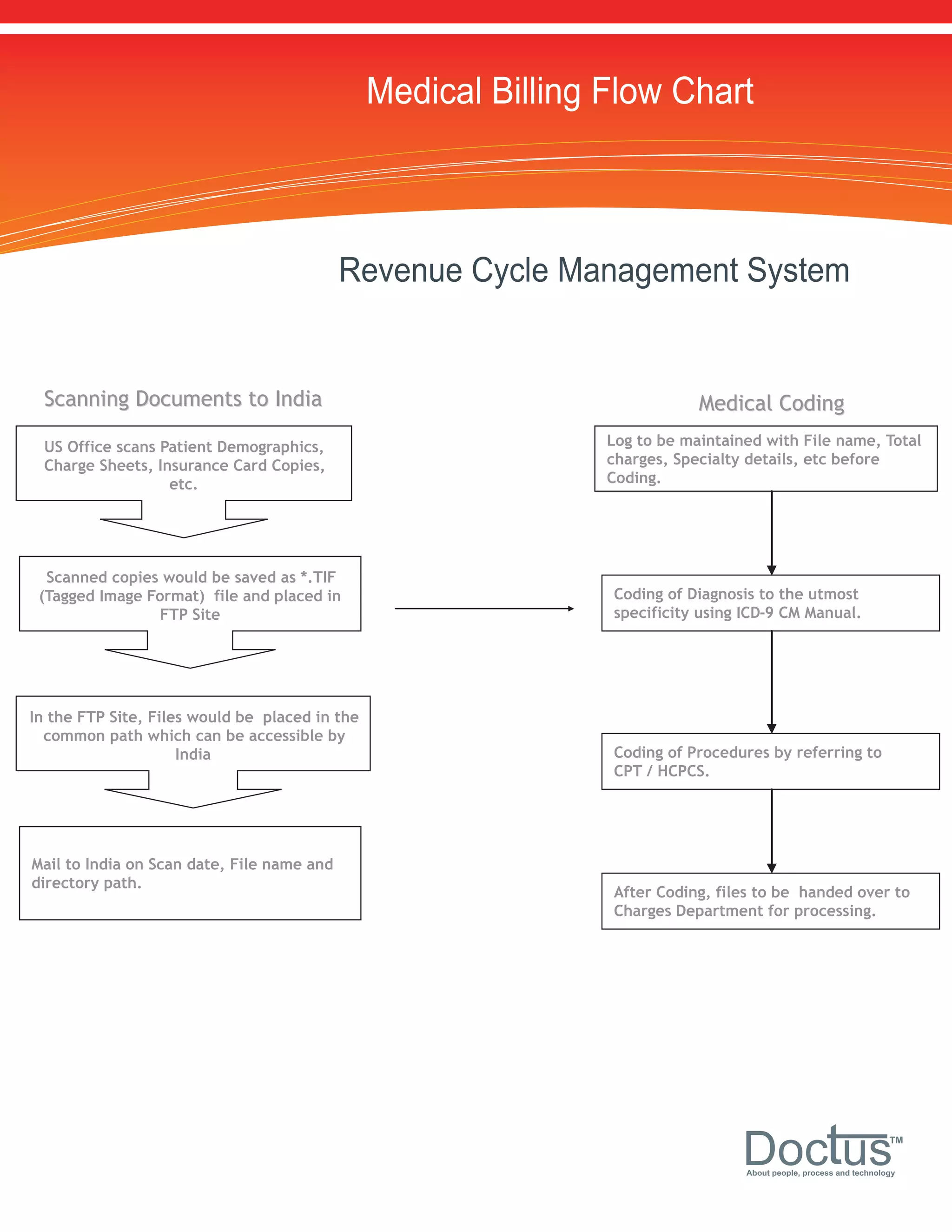
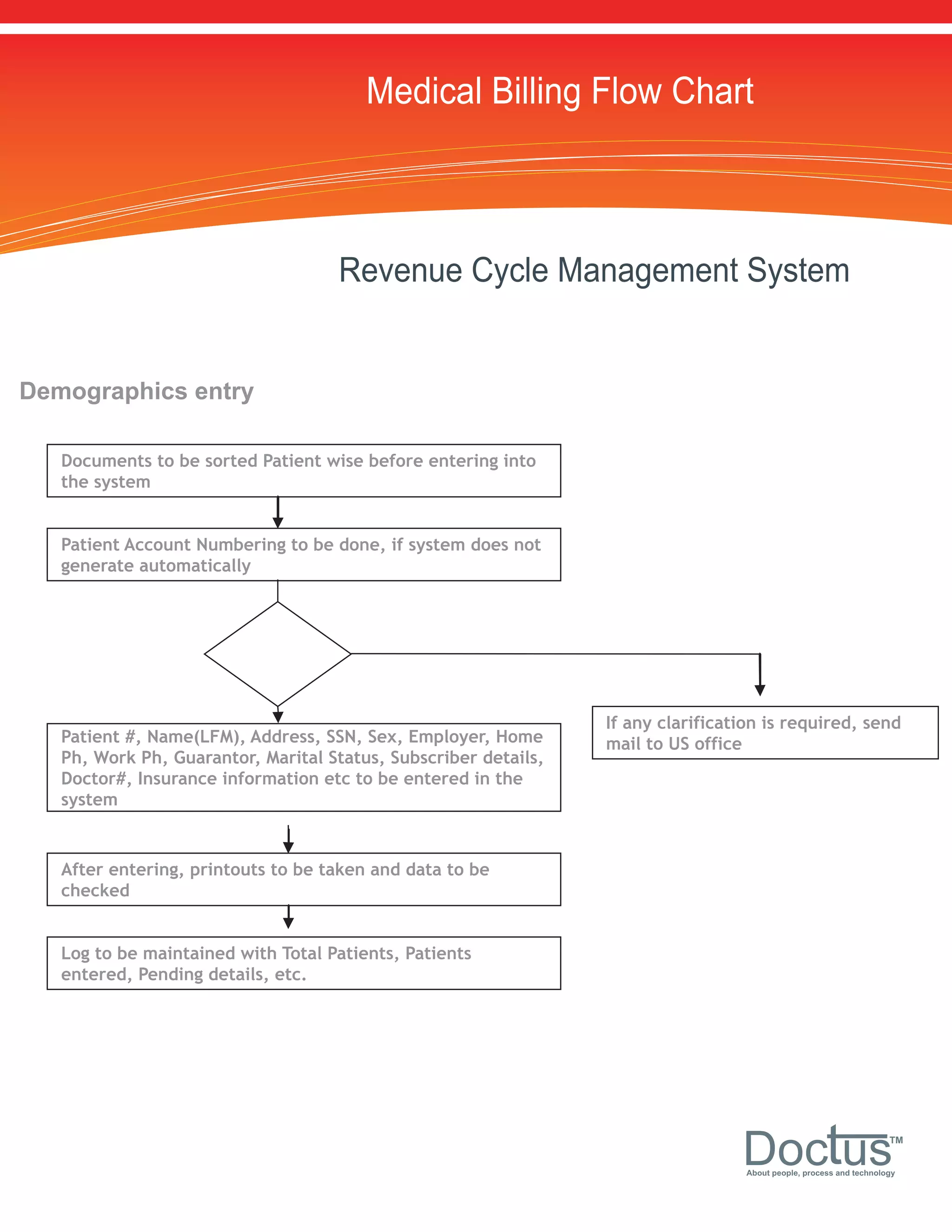
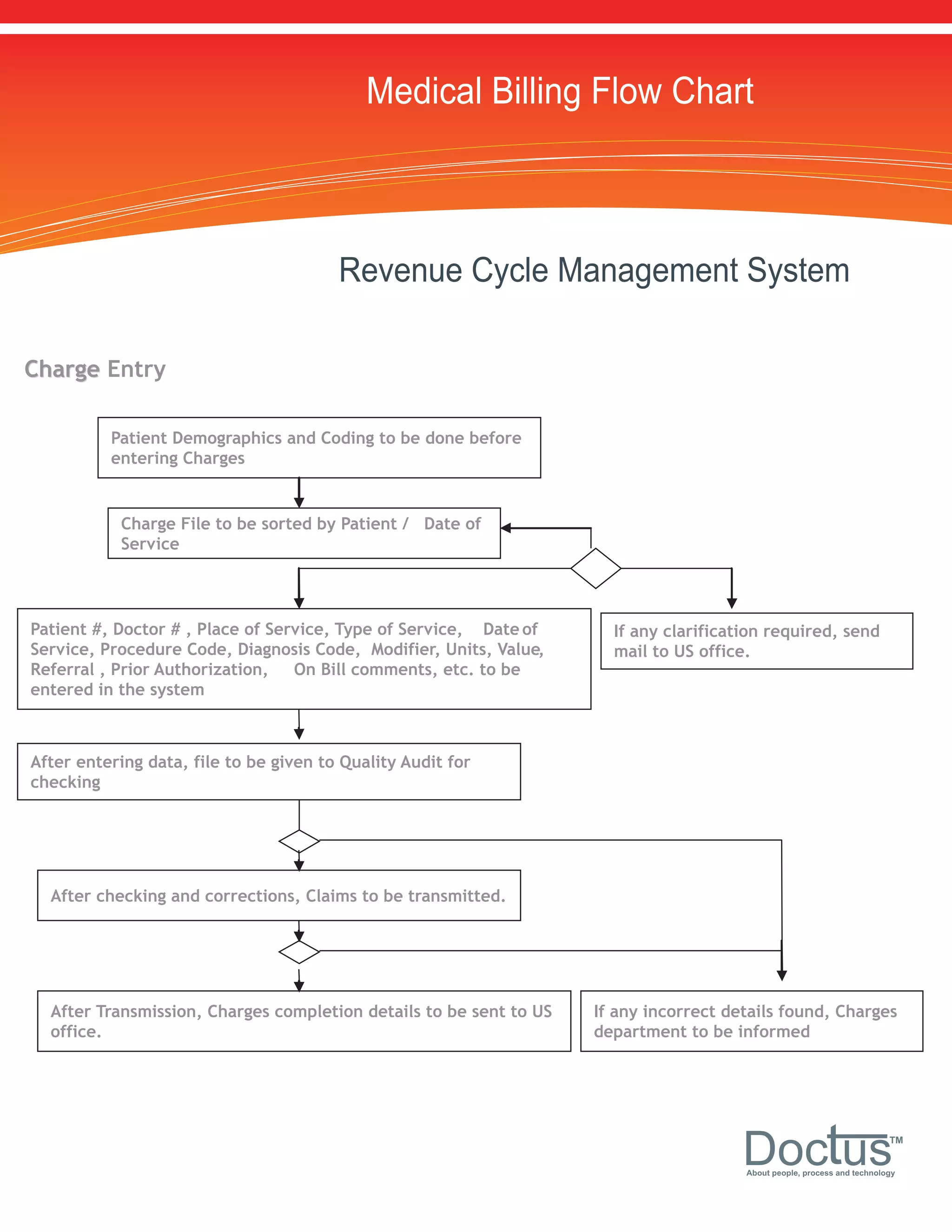
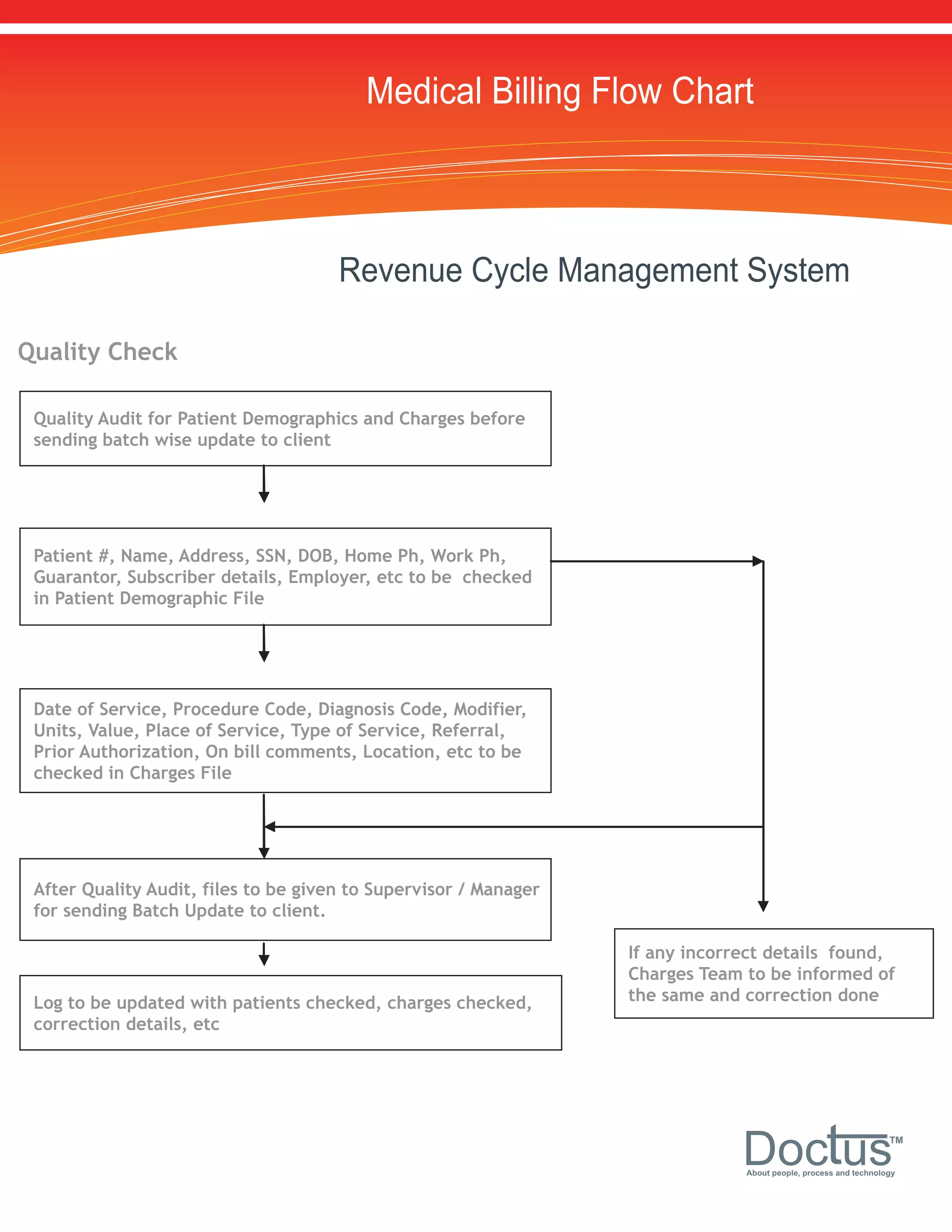
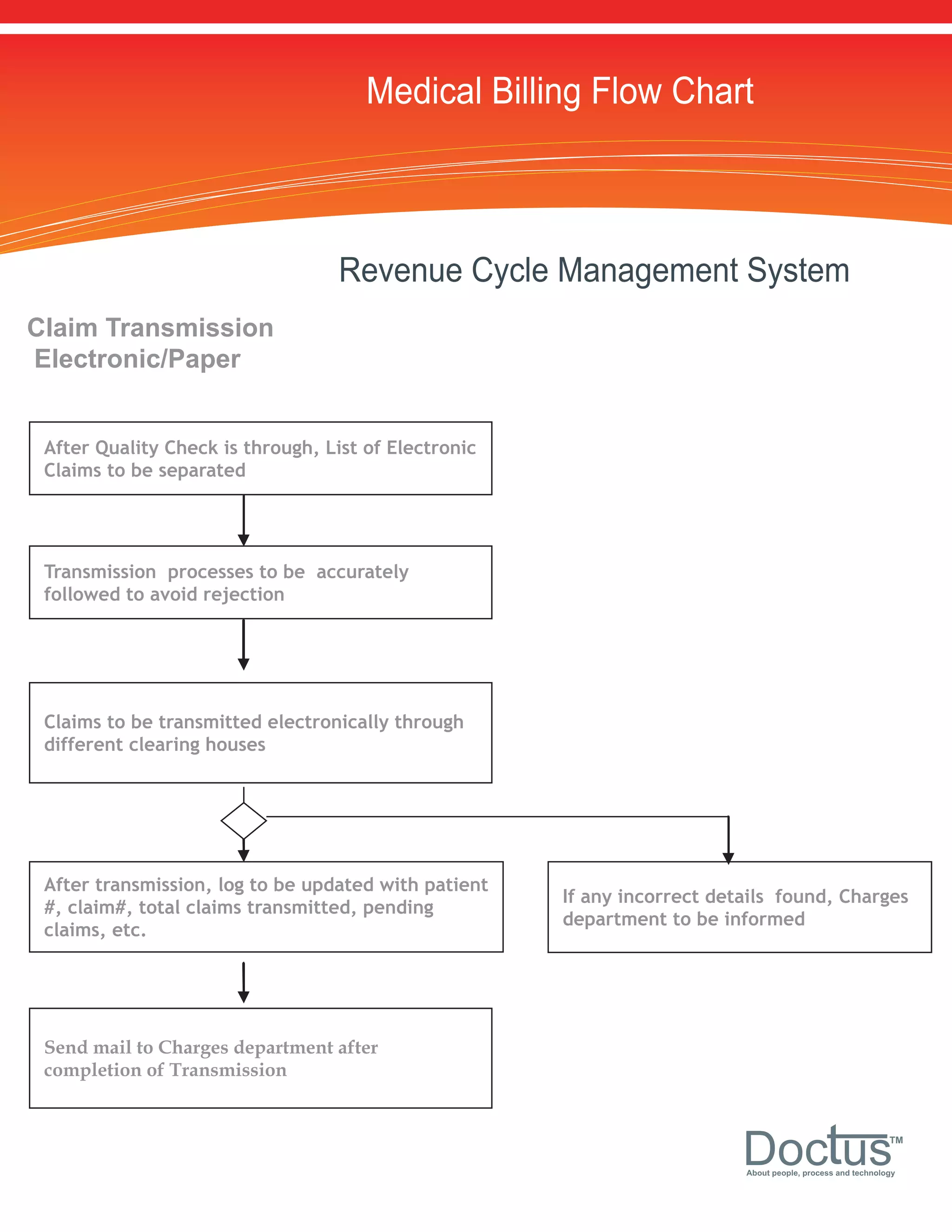
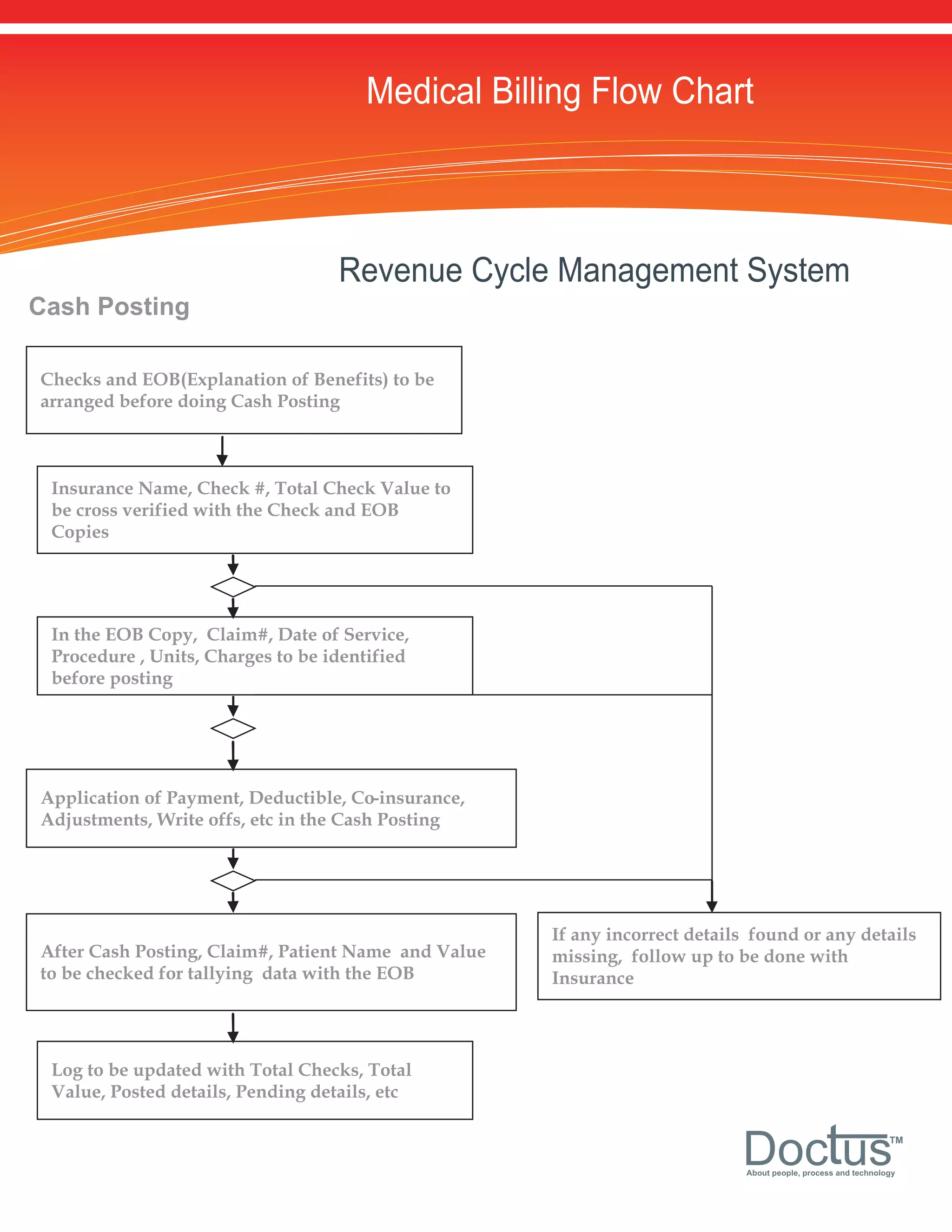
The document outlines the medical billing flow chart and revenue cycle management system. It involves verifying patient eligibility, coding medical records, entering demographic and charge data, transmitting claims to clearinghouses, receiving explanations of benefits (EOBs), posting payments, and following up on denials to increase collections. Key steps include eligibility checks, coding, data entry, quality audits, transmission, cash posting, and accounts receivable management.