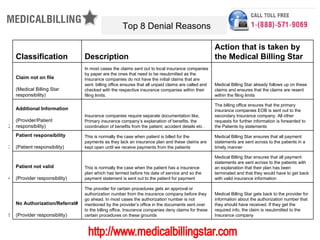
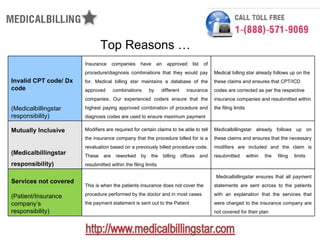
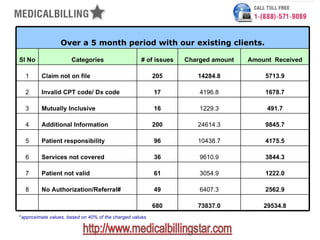
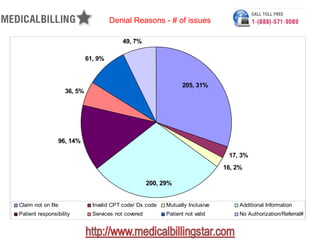
The document outlines the top eight reasons for claim denials in medical billing, including issues such as claims not on file, invalid codes, and lack of authorization. It details the actions taken by the billing office to address these issues and specifies the responsibilities of both patients and providers. Additionally, it provides statistical data on denial cases and amounts charged and received, emphasizing the importance of effective denial management in minimizing lost revenue.