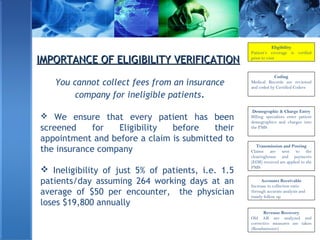
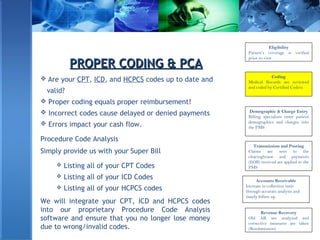
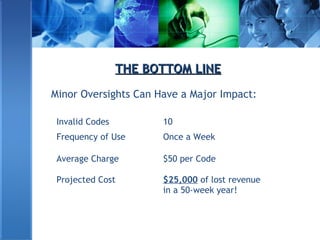
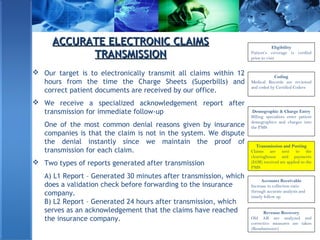
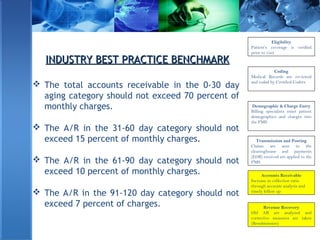
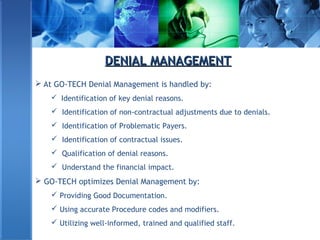
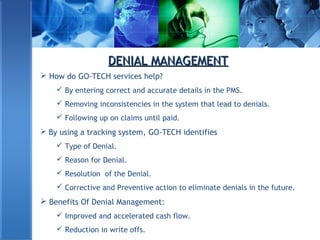
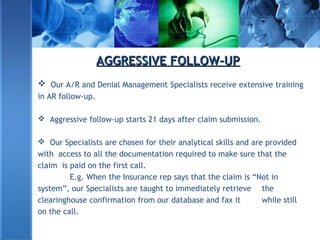
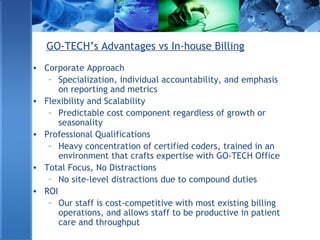
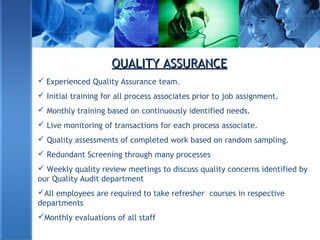
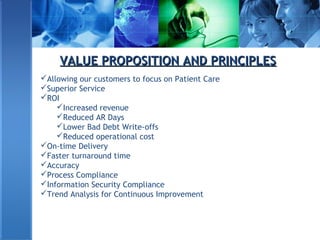
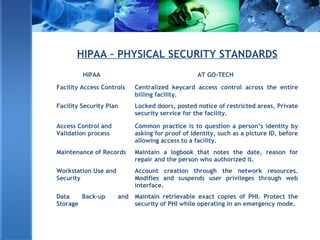
Go-Tech offers HIPAA compliant revenue cycle management services, including medical transcription, coding, billing, and denial management for healthcare providers. The company emphasizes accuracy in claims processing and denial management to optimize cash flow for physicians and hospitals. Their professional team and state-of-the-art technology ensure high service levels and cost containment, helping clients reclaim their rightful revenue from insurance companies.