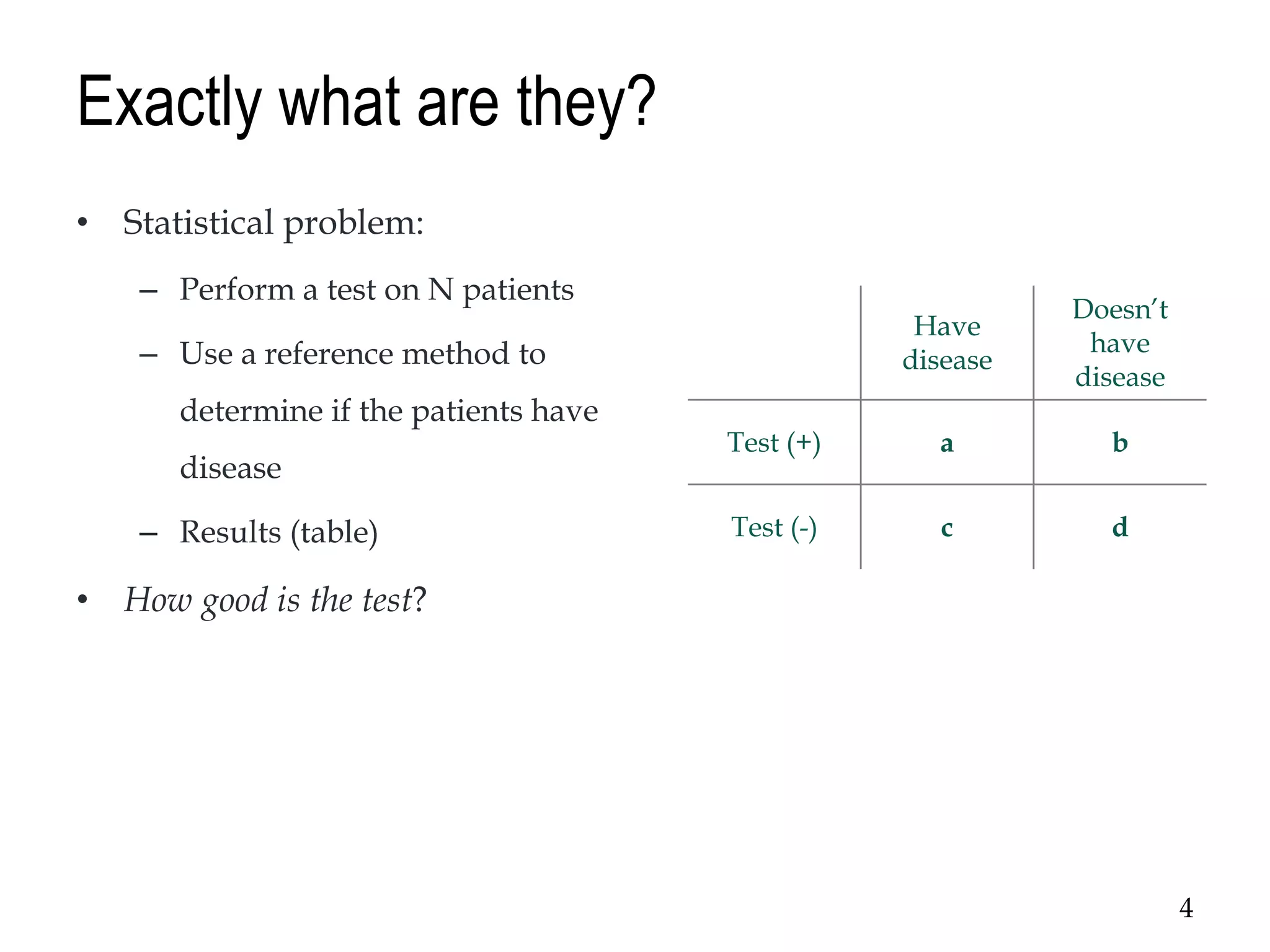
The document discusses diagnostic accuracy in clinical settings, focusing on sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of diagnostic tests, particularly for HIV. It highlights how these parameters depend on disease prevalence and emphasizes the utility of likelihood ratios for ruling in or out diseases. The presentation also incorporates examples and references to support understanding of diagnostic performance measures.