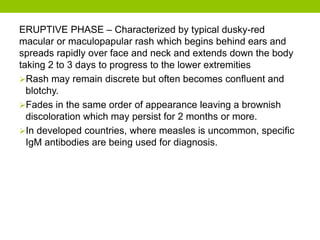
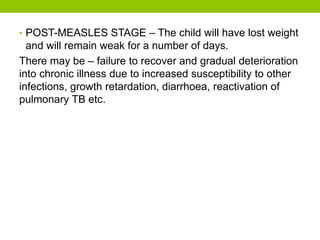
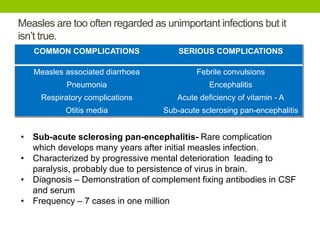
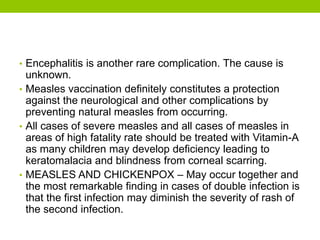
Measles is a highly infectious disease caused by a virus. It begins with fever and respiratory symptoms and causes a characteristic rash. While usually mild, it can lead to serious complications like pneumonia or encephalitis. Measles is prevented through the measles, mumps, and rubella (MMR) vaccine, which is recommended as two doses for children, with the first between 9-15 months. Vaccination has greatly reduced measles cases and is the best way to protect against this still common disease globally.