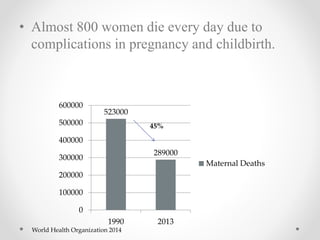
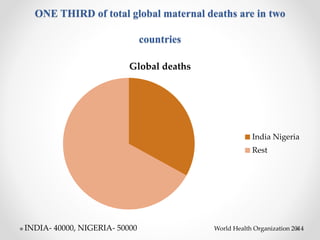
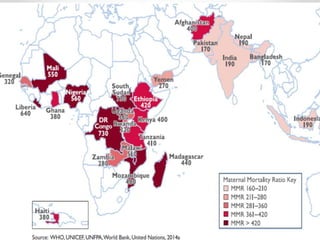
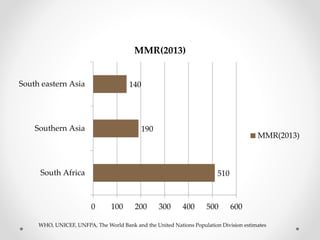
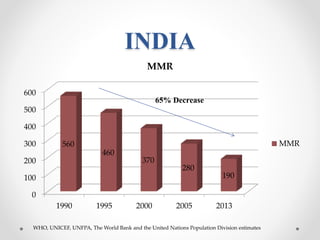
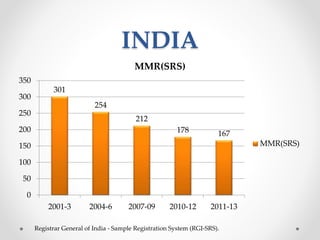
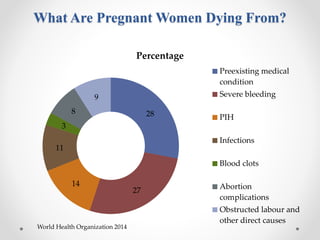
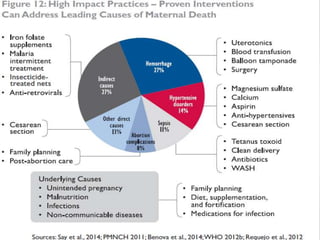
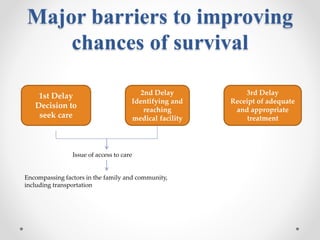
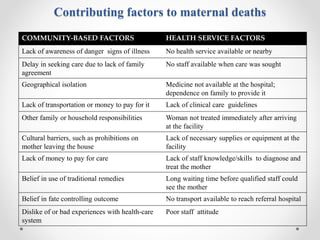
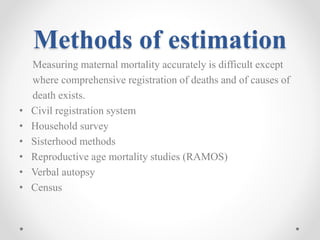
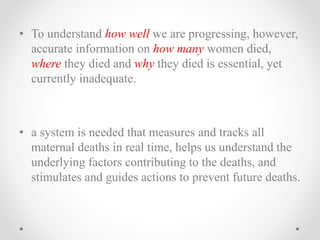
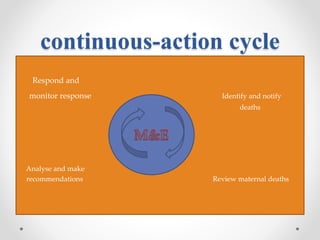
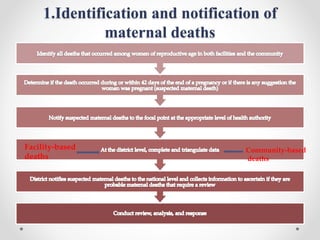
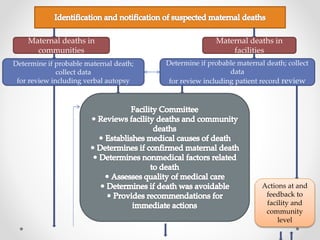
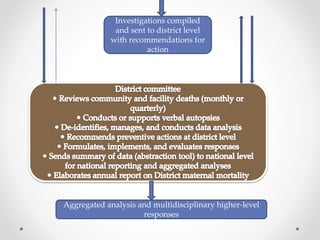
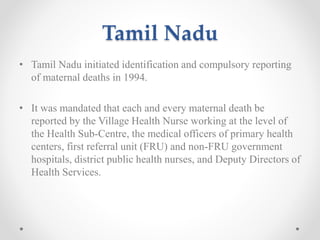
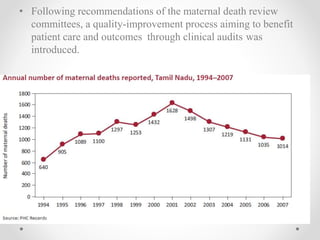
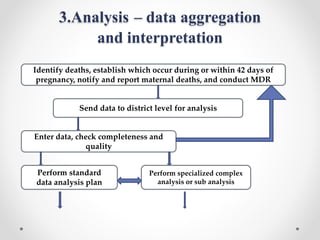
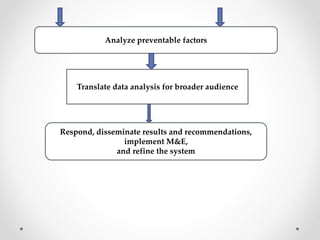
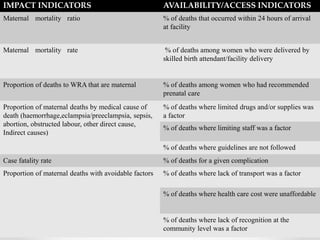
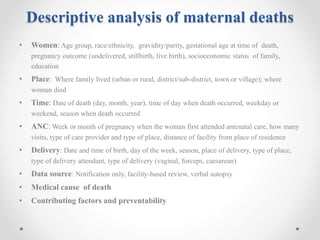
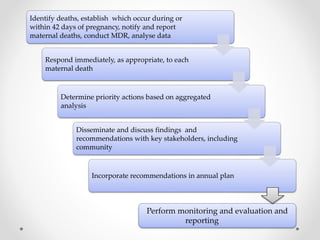
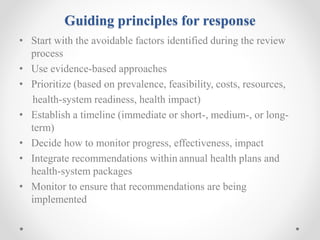
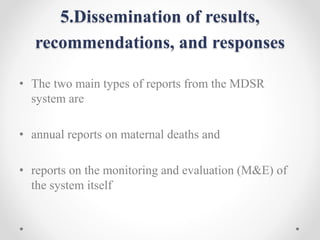
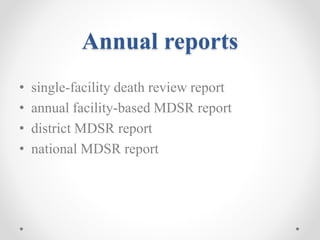
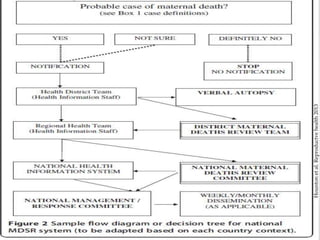
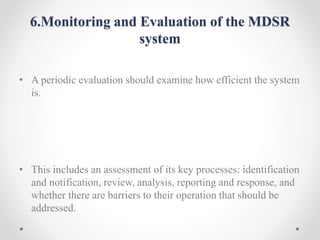
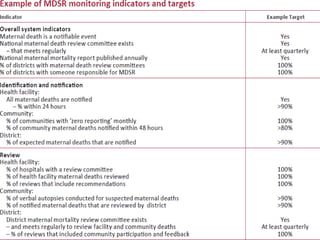
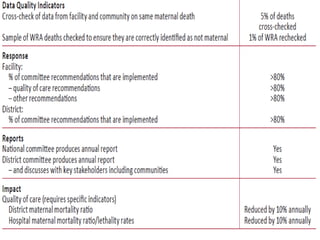
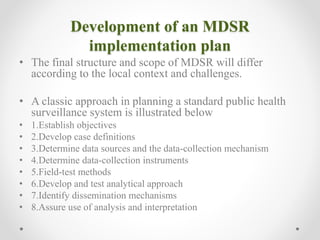
This document discusses maternal death surveillance and response (MDSR) in India. It provides definitions of key terms like maternal mortality ratio and describes the current state of maternal deaths globally and in India. The document outlines the goals and steps of MDSR, which includes continuously identifying and reviewing maternal deaths to understand causes and barriers in order to take actions to prevent future deaths. MDSR aims to eliminate preventable maternal mortality by linking information gathered from reviewing deaths to immediate and long-term responses.