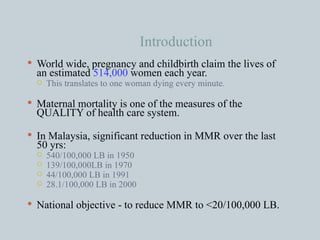
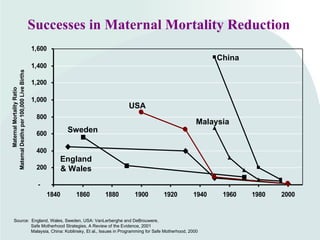
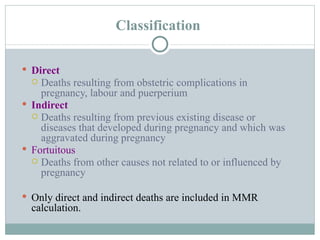
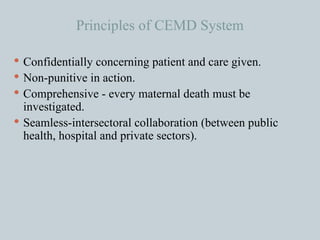
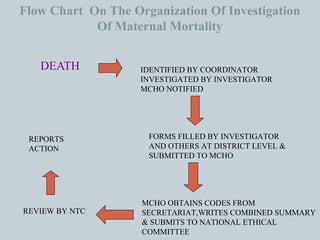
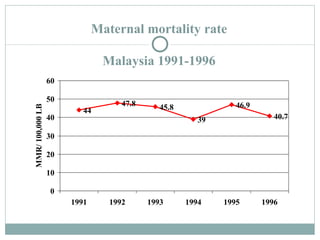
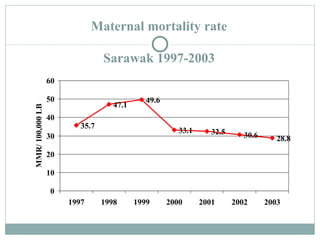
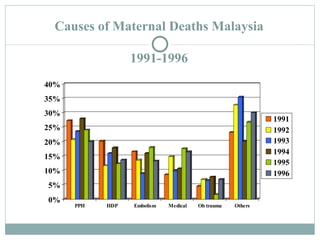
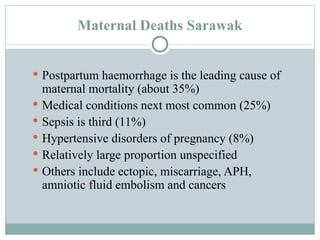
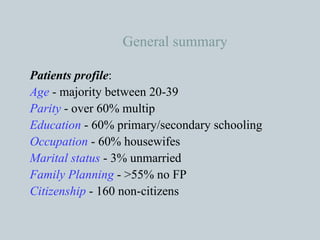
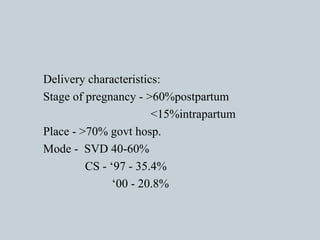
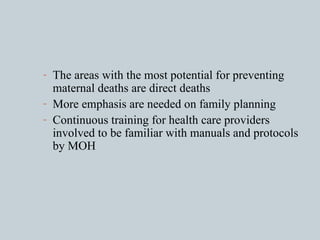
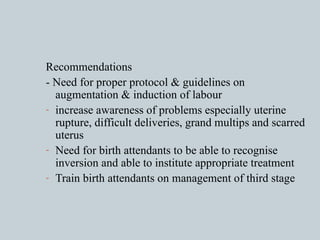
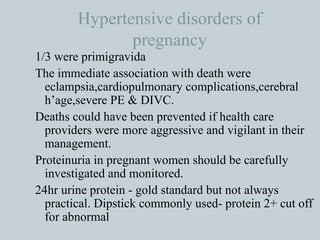
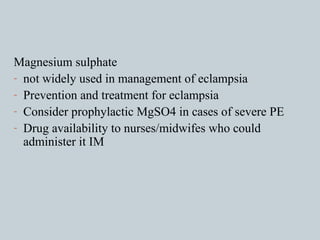
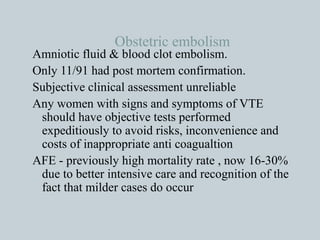
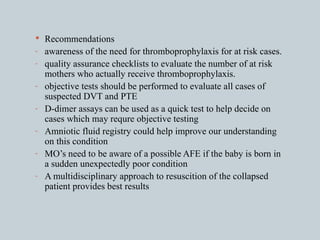
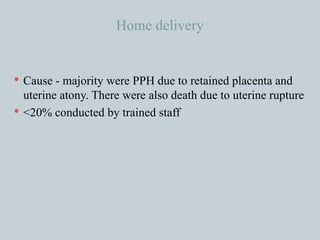
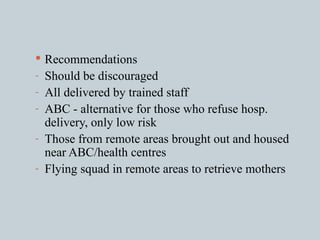
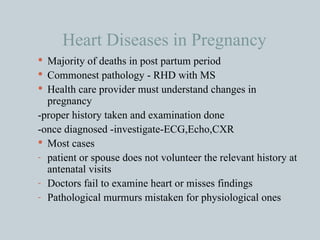
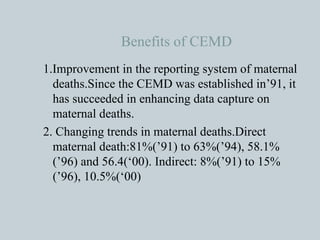
Maternal mortality remains a significant issue worldwide, with over 500,000 deaths annually. Through initiatives like the Confidential Enquiries into Maternal Deaths system, Malaysia has significantly reduced its maternal mortality rate from 540/100,000 live births in 1950 to 28.1/100,000 in 2000. Postpartum hemorrhage is a leading cause of death in Malaysia, while medical conditions, sepsis, and hypertensive disorders also contribute substantially. Recommendations focus on increasing access to emergency care and transportation, improving provider training, and expanding family planning programs.