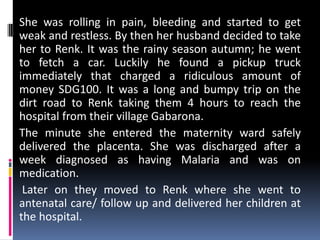
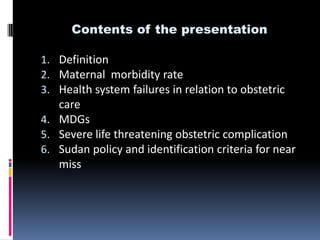
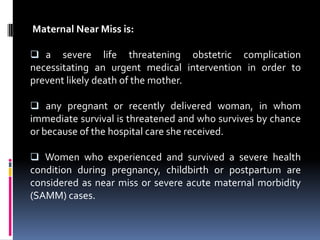
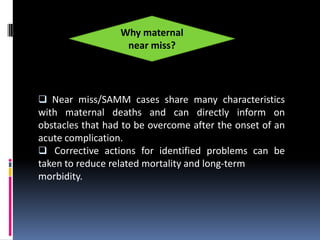
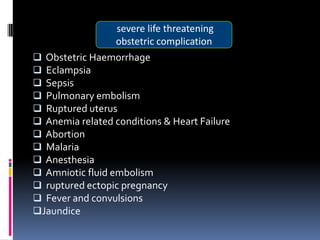
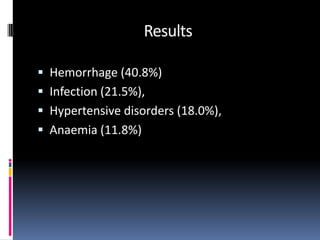
This document summarizes presentations on maternal near miss in Sudan. It defines maternal near miss as a severe life-threatening complication during pregnancy, childbirth, or postpartum that requires urgent intervention to prevent death. The document discusses how analyzing near miss cases can provide insights into health system failures in obstetric care. It notes that the leading causes of near miss in Sudan are hemorrhage, infection, hypertensive disorders, and anemia. The document also outlines Sudan's policy on identifying near miss criteria and qualitative research examining determinants of maternal morbidity and mortality in post-conflict areas.

![Method
Qualitative study design using Critical Incident
Technique [CIT].
11 near miss events.
Interviews were conducted with husbands,
mothers, in laws, sisters, midwives of the
deceased and in case of survival the maternal
near misses.](https://image.slidesharecdn.com/mternalnearmiss-120825132949-phpapp01/85/Maternal-near-miss-20-320.jpg)