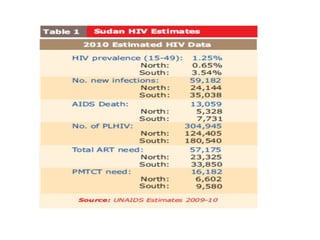
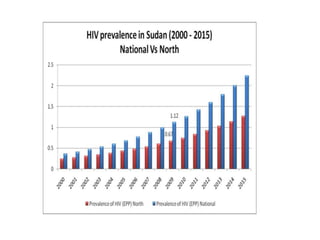
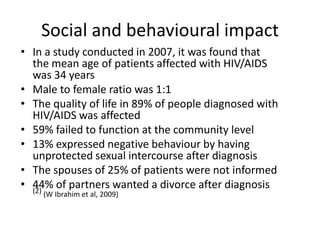
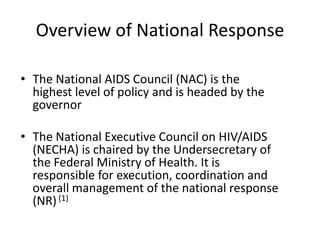
HIV/AIDS prevalence in Sudan is estimated at 600,000 people, with the first case reported in 1986. The Sudan National AIDS Control Programme was established in 1987 to coordinate the national response. Key challenges include limited funding, poor surveillance, and low access to treatment, prevention, and HIV testing services due to stigma. Expansion of programs for mother-to-child transmission prevention, blood safety, and care for at-risk groups is needed to improve Sudan's national HIV/AIDS response.